Speakers at the ESTRO 2024 meeting discussed the potential for upright treatment to increase global access to radiotherapy, particularly particle therapy

Upright radiotherapy, in which a patient is treated in an upright position rather than lying down (supine), is an old technique that’s seen a resurgence of interest recently. At the ESTRO 2024 meeting, experts in the field discussed the potential benefits and ongoing challenges of upright radiotherapy – in a quest to discover whether the approach offers hope or is merely hype.
Up first, Ye Zhang from PSI took a look at some of the key driving forces for moving to upright radiotherapy. The ability to rotate and reposition the patient during upright treatments removes the need for a costly and bulky gantry. And eliminating the gantry reduces the space requirements for a particle therapy system by an estimated 80%, greatly lowering the costs of installing a treatment facility.
“Reducing the cost increases the accessibility of particle therapy to the population worldwide,” Zhang explained, citing a recent review paper that concluded “only 1% of radiotherapy patients currently receive particle therapy, however, at least 15% of patients could benefit”.
As well as offering economic advantages, removing the gantry provides more space at the isocentre, enabling the integration of advanced treatment methods such as proton arc therapy, combined proton–photon treatments and the use of MR guidance.
Upright treatment could increase patient comfort, reduce proton therapy costs
Upright positioning may also provide clinical advantages, by utilizing geometric variations between the target and the organs-at-risk to distribute dose. The idea here is that different organ positions, morphology and motion directly affect the dose distribution and may provide a means to optimize radiation delivery.
“The potential for upright treatment is significant,” Zhang concluded. “Not only to reduce the cost, which is important to push particle therapy worldwide to benefit more patients, but it also has potential clinical benefits which are under investigation, and there’s definitely a lot of potential to integrate future advanced radiotherapy concepts.”
Work in progress
While upright radiotherapy offers many potential benefits, there are still ongoing challenges to solve. “Upright radiotherapy is a true paradigm shift because it affects every step in the workflow: imaging, segmentation, treatment planning, quality assurance, treatment delivery and even follow up,” explained Lennart Volz from GSI. “All of these steps have to be translated into the upright position.”
Volz pointed out that upright treatment is not a new concept, with investigations into chair-based solutions dating back to the 1960s. “Yet, to the best of my knowledge, there are currently only six centres treating in an upright position, for indications other than ocular tumours,” he said. “On the other side, there are 110 gantries.”
One reason behind this slow uptake may be a previous lack of commercial upright imaging systems, as well as the absence of modern tools such as adaptive workflows and image guidance. Nearly all body sites will undergo anatomic changes between supine and upright postures, making upright planning-quality CT essential for clinical transfer. Upright MRI and PET systems may also be needed. Luckily, said Volz, several industry vendors are now developing cost-efficient upright imaging systems.
For image segmentation, one unknown is whether existing auto-contouring tools trained for supine treatments still work for upright geometries. Treatment planning and quality assurance (QA) procedures may also require modification, with new margin recipes and bespoke QA equipment, for example. It’s also important to define which upright posture (straight, leaning forward, half standing, for instance) is best suited for each treatment site. Finally, Volz emphasized that an adaptive workflow is mandatory.
“Upright radiotherapy has a lot of potential, but many challenges remain,” he concluded. “The most crucial challenge is that we need more data, more evidence to support the different decisions that have to be taken for upright radiotherapy. Luckily, there are many ongoing projects in the field to address these challenges.”
Early experience
Sophie Boisbouvier of Centre Léon Bérard examined upright treatment from the patient’s perspective, sharing her experience of using the upright positioner developed by Leo Cancer Care. In one example, a study of nine breast cancer patients who spent 40 min in the positioner, seven of the participants preferred the upright to the supine position.
In another study, 16 pelvis cancer patients were setup three times in the upright positioner for comparison with supine treatment. In the supine position, some patients reported pain and found it difficult to be setup or get out; this was not the case for the upright position. “Globally, patients seem more comfortable and more satisfied in the upright position than the supine position, or at least as comfortable and as satisfied,” she said.
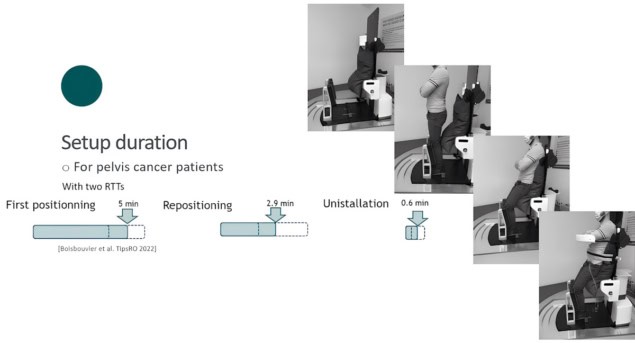
For these 16 patients, initial positioning took 5 min (with two radiation therapy technologists), repositioning less than 3 min and uninstallation less than 1 min. The mean inter-fraction positioning shift was below 1 mm in all directions. And after 20 min on the chair and several rotations, the mean position shift was close to 0 mm.
“It seems feasible to setup a patient in a reasonable time frame, but we still need additional data and comparison with data on the supine position,” she said. “For reproducibility and stability, the first data are promising, however, we also need more data on various localizations and 3D images to know whether the organ position is reproducible and stable.”
At the Northwestern Medicine Proton Center in Chicago, there’s a fully clinical upright system that has already treated over 675 patients. Mark Pankuch explained that the four-room proton centre has one gantry, one fixed beam and two inclined beams that offer two treatment positions. When the gantry reached full capacity, “we wanted to go to upright treatments, because we needed more gantry-type treatments and only had one gantry system,” he said.
To achieve the move to upright, the group first needed an upright imaging system. They collaborated with system vendor P-Cure to install a wall-mounted CT scanner that lowers itself vertically over the patient. The next task was to design a positioning chair that was compatible with the treatment room’s existing robotic systems.
Due to limitations in the robot’s vertical movement, they ended up designing two chairs: one optimized for the thorax and the other for cranial treatment. The centre now treats about 80 patients per year, the majority in the cranial chair. To date, 57% of these have been ophthalmic treatments and 29% brain or spinal cord treatments.
“Lots of lessons were learned, but the one big takeaway is that we designed a scanner and a chair for an existing room for a particular need,” Pankuch explained. “If a treatment room was designed around an ideal scanner or chair, there’s much more utility, functionality and efficiency that can be gained for sure.”
Strategy and enthusiasm
Rounding off the symposium, Thomas Bortfeld from Massachusetts General Hospital described some advanced treatment concepts facilitated by upright radiotherapy. Advances in beam geometry could enable particle therapy to fit into a conventional treatment room of about 50 m2, giving more patients access to this treatment.
Increasing delivery speed, meanwhile, allows more patients to be treated in a single clinical centre. Currently, the main speed limiting factor is the switching between energy layers, which can account for over 70% of the delivery time. “Once we simplify our beamlines in the upright scenario, we can maybe get away with much simpler beamlines that will reduce the energy switching time to essentially zero,” Bortfeld said, adding that his colleague Konrad Nesteruk and international collaborators are currently investigating fixed-field alternating gradient techniques that remove the need to switch the magnet for different energy settings.

Patient positioning chair paves the way for upright radiotherapy
Image guidance remains a key challenge for upright radiotherapy. Bortfeld’s group is currently studying ultralow-field MR guidance using a mobile 64 mT scanner, which they are about to test in the proton environment. They are also testing 6.5 mT MRI for breast imaging, finding that even this extremely low field provides decent image quality.
As for the symposium’s theme of hope versus hype, Bortfeld thinks there is a little bit of both. “Hype is not what we want, but it’s good to see a lot of interest. There certainly is also hope, no question of that,” he concluded. “What we really need is not hype but enthusiasm, and many of us have enthusiasm in this field. We also need, maybe not only hope, but to define a strategy. Strategy and enthusiasm is where we want to be.”



