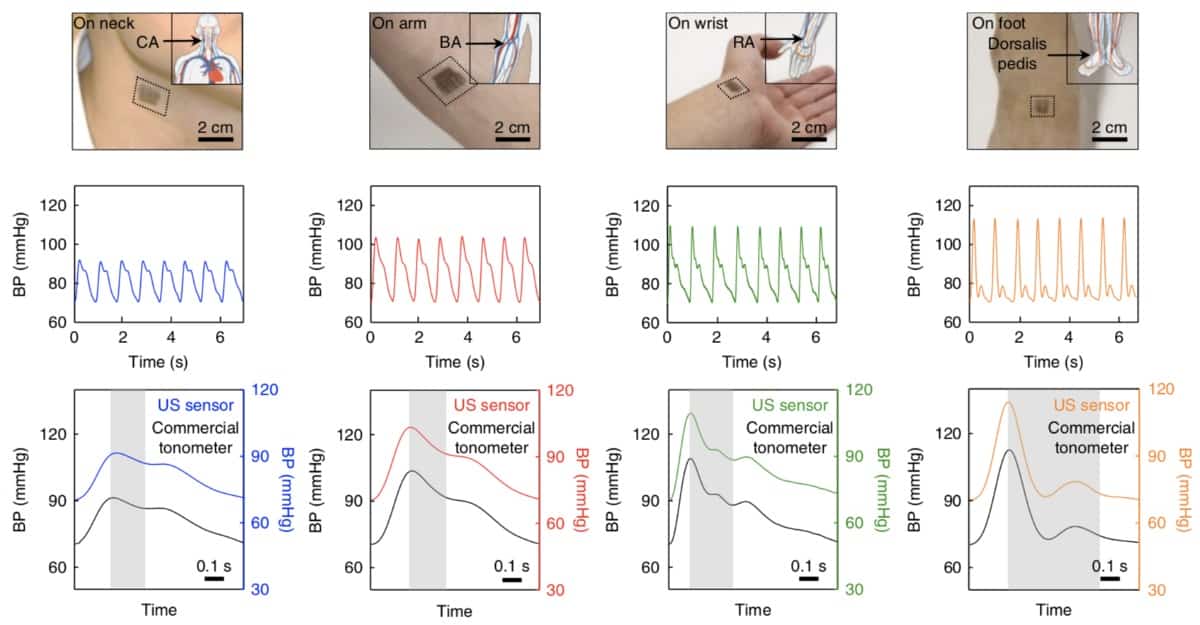
A wearable patch, designed by Sheng Xu’s research group at the University of California San Diego, can flex and conform to the skin’s surface while assessing blood pressure (BP) through ultrasonic waves. It performs as well as other non-invasive methods used to measure BP without presenting their associated caveats (Nature Biomed. Eng. 2 687).
By measuring the pulsatile behaviour of the artery diameter, the patch can derive pressure in real time and yield important predictors of related cardiovascular events. For example, when combined with an electrocardiogram sensor, the patch can assess the speed at which the blood pulse wave travels along the arterial tree. This is an important feature of hypertension, as stiffer arteries lead to high velocities.
The patch is only 240 µm thick and is composed of a 4×5 array of tiny rigid piezoelectric transducer elements that emit a 7.5 MHz ultrasonic wave, combined with soft structural components such as meandering stretchable electrodes. The whole assembly is encapsulated within a silicone elastomer so that its elastic modulus matches that of the skin.
The best of both worlds
BP is routinely measured around the world to inform doctors’ clinical decisions. But the BP cuffs that they use only give landmark values, such as maximal (systolic) and minimum (diastolic) BP, not the whole BP waveform, which contains more comprehensive information for diagnosis and prognosis.
The gold standard for assessing the entire BP waveform is invasive, as it requires insertion of a catheter into the site of interest. Thus non-invasive alternatives were developed — but their shortcomings limit their use to research purposes.
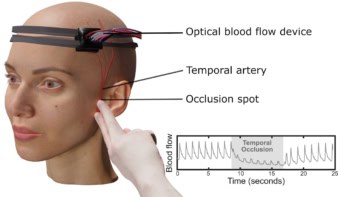
Photoplethysmography, for example, links BP to light absorption, but it can only be used on a shallow vessel, such as in the finger. Tonometry, meanwhile, in which a sensor records the vessel pulsation and wall motion tracking of the artery with ultrasound, can only be performed by a skilled operator. Tonometry also requires a supporting bone beneath the artery flattened by the sensor; and wall motion tracking is vulnerable to motion artefacts from respiration and shaking by both patients and operators.
Wearable devices offer autonomous, non-invasive, continuous monitoring of many signals (temperature, sweat content, skin hydration, etc). The incorporation of ultrasonic probes allows investigation of deeper phenomenon that are currently inaccessible by existing wearable devices.
The importance of central BP
This work also brings into sharp focus the prevalence of central BP, the pressure near the heart, over peripheral BP assessed from distal locations (brachial or radial arteries in the arm). Historically, the first BP measuring devices assessed the latter; but recent findings led to a paradigm shift. The rationale for this was that central BP is more representative of the force that major organs such as kidneys or the brain are exposed to. Studies revealed that peripheral BP could be up to 20 mmHg higher than central BP, due to amplification phenomena caused by pulse wave propagation and reflection.
Mathematical techniques exist to transform peripheral into central BP, but BP-lowering drugs can have different effects at these two locations, leading to inaccurate estimates. More importantly, these mathematical tools are not patient-specific, but result from observations in selected cohorts of patients that were then generalized.
By allowing real-time monitoring of patient-specific information regarding central BP, without requiring external assistance, the new patch can usher BP monitoring in a new era in which the whole BP waveform is used to assess a patient’s health, instead of just diastolic and systolic BP.
The next steps for the technology involve integrating a wireless compound to transfer data from the patch to a monitor and process the data to deliver the relevant information to the doctor. The researchers are currently looking for collaborators to carry out these improvements.