Spotting dangerous electrical activity in the heart and refining radiation doses in cancer therapies were among the topics discussed today at a conference on Simulation and Modelling Applied to Medicine. Organized by the Institute of Physics, the forum highlighted the growing role of physics in the high-tech world of medicine.

The beating of the heart is controlled by a wave of electrical activity that starts at the sino-atrial node – the heart’s natural pacemaker – and spreads outwards. In a healthy heart each wave has faded away by the time the next wave arrives. But if this does not happen, it can lead to a heart attack. Understanding this process – which is known as ventricular fibrillation – is the key to developing new ways to treat the victims of cardiac arrest.
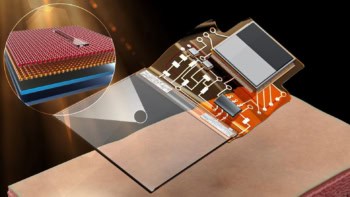
Richard Clayton of the University of Leeds and co-workers at the University of Auckland in New Zealand have developed a computer simulation that shows the electrical patterns in the heart when these faulty beats occur, as shown in this image. Also shown are the ‘filaments’ that the unstable ‘re-entrant’ waves rotate around. ‘Our detailed biophysical and anatomical model can simulate this activity’, says Clayton, “and we can then test different pharmacological and physical treatments that could help the patient’.
In the field of radiotherapy, two teams of scientists have devised models that should make treatments safer and more efficient. Norman Kirkby of the University of Surrey worked with engineers and cell biologists from Addenbrooke’s Hospital in Cambridge and Mount Vernon Hospital in Middlesex to simulate the multiplication of cancer cells in brain tumours. The growth of such tumours can be stopped if the DNA in these deviant cells is damaged by doses of radiation.
When cancer cells multiply, they go through a cycle that includes a ‘self-checking’ stage. If the tumour is irradiated during this period, the cells simply repair the damage and keep growing. But the model devised by Kirkby’s team could enable doctors to track the cycle so that they can administer radiation treatments at accurate intervals. This means that the cancer cells will be hit when they are most vulnerable, and damage to healthy tissue will be minimized.
Meanwhile, Frank Verhaegen of the National Physical Laboratory and – working independently – Emiliano Spezi at Velindre Hospital in Cardiff have developed Monte Carlo simulations to calculate optimum radiation doses for individual patients. Existing models for calculating such doses are based on simplified physical models and can overlook the different responses of bone and soft tissue to radiation, which may lead to an inaccurate dose.
The Monte Carlo methods developed by Verhaegen and Spezi predict the paths of every particle as it travels from the accelerator and into the patient. This should allow doctors to account for the exact anatomy of each patient when calculating their radiation dose.