The days of pricking fingers several times a day to draw blood could become a thing of the past for diabetes sufferers, thanks to a new way of monitoring sugar levels in the body. The minimally invasive test, developed by researchers in Japan, could also provide patients with a more detailed picture of glucose concentrations as they fluctuate over time.
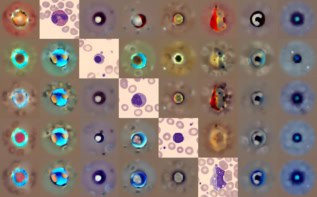
Shoji Takeuchi and his colleagues at the University of Tokyo, working with collaborators in industry and at Kyoto University Hospital, have developed a type of fluorescent bead that can be injected into skin. The beads contain a type of boronic acid that binds reversibly with glucose molecules. Once inside the blood, these beads, which are of the order 1 × 102 µm, can be tracked to reveal blood sugar levels by exposing skin to light.
In practice, diabetic patients would need devices containing an excitation light source and photodiode to read out the fluorescent signal. “The device would be as small as a watch or a piercing, and diabetic patients would wear the device,” Takeuchi tells physicsworld.com.
Glowing hair
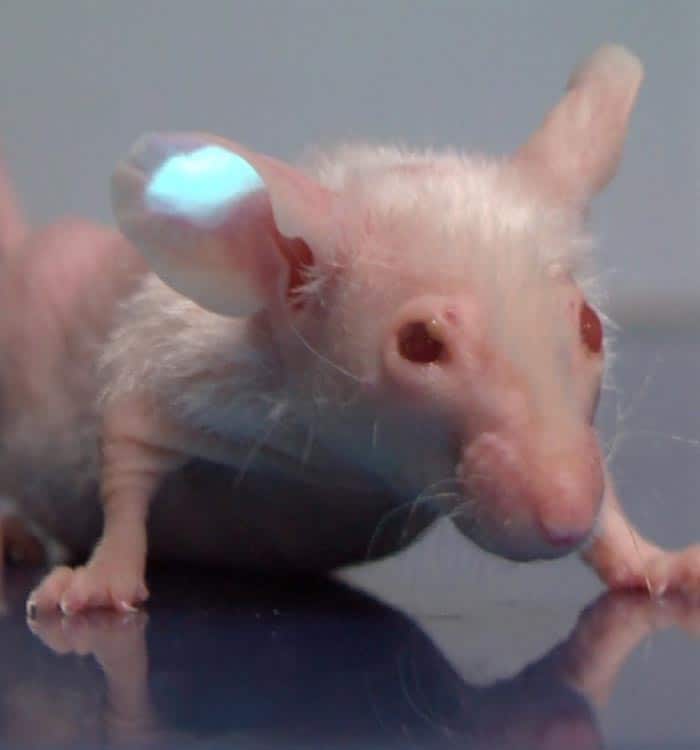
In a series of in vitro tests, the researchers observed the relative fluorescence increase by five times as they raised glucose concentrations from zero to 1000 mg.d/L. They also carried out a series of in vivo tests by injecting their fluorescent beads into the ear skin of a mouse using a needle commonly used in clinical settings. The implanted beads were still visible through skin layers thicker than 200 µm even when impeded by hair.
Takeuchi believes that the technique could become commercialized within five years but there are still aspects of the science that need to be developed before it can be taken to a clinical trial. “For the next step, we are going to improve the microbeads so they have a little protein adsorption – this is important to keep the microbeads performing stably in a body,” he explains.
Ishan Barman, an analytical chemist at Massachusetts Institute of Technology, is impressed by the breakthrough. “The real highlight of this sensor is its capability to provide high intensity levels that leads to sensitive detection, even for transdermal monitoring,” he says.
Outstanding challenges
But Barman also realizes that there are several remaining challenges. “Since this is a minimally invasive design (as opposed to a non-invasive one), one has to further explore the material toxicity question, especially in human population.” Barman also notes that the researchers need to examine how the particles clear from the body over days and weeks, not just hours.
This research joins a number of other innovations that could come provide diabetes sufferers with an alternative to the “finger prick” test. These techniques could provide a more immediate and continual response to changing glucose levels in blood, as opposed to taking blood samples, which only provides a snapshot in time. Examples include the carbon “tattoo” containing nanotube sensors and a non-invasive Raman spectroscopy technique, both techniques being developed at MIT.
The work of Takeuchi and his colleagues is described in a recent paper in Proceedings of the National Academy of Sciences.