The Lorentz force combined with acoustic shear waves could help doctors detect dangerous diseases, say researchers in France. The team has shown that the electromagnetic force could create oscillations in living tissue, producing shear waves that can be detected to reveal the tissue’s elasticity. The technique has shown promise in the laboratory and could now be developed as a clinical technique.
An experienced doctor can determine a lot about the human body by simply pressing on it with their fingers, a process called palpation. Many serious medical conditions such as breast cancer can be diagnosed this way because they cause tissue to be firmer than normal. Some internal organ diseases such as liver fibrosis also cause the tissue to stiffen, but, in general, these organs are inaccessible to manual palpation. While the texture of internal tissue can be probed by medical imaging techniques such as ultrasound, these techniques measure a different quantity from palpation.
Shear propagation
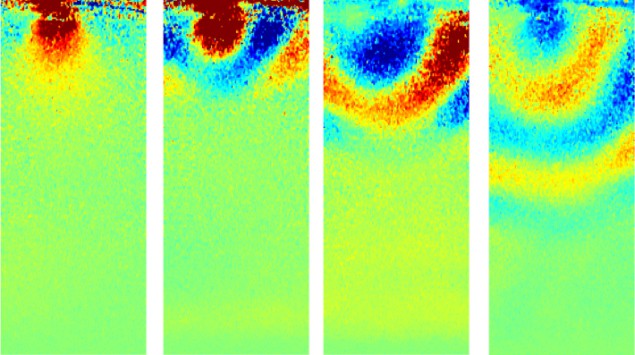
When tissue oscillates, it supports both pressure waves (back-and-forth motion) and shear waves (side-to-side movement). Traditional ultrasound techniques operate in the megahertz range and at these frequencies shear waves propagate just a few microns in tissue. As a result, most ultrasound techniques rely on using pressure waves to determine the compression modulus of the tissue.
However, tissue is mainly water – an incompressible fluid – so its firmness to the touch depends on how easily it moves aside to allow a doctor’s fingers to sink in. This is defined by the shear modulus, which can be calculated from the speed of the shear waves in the tissue. Therefore, measuring the sheer modulus can give doctors a map of the inside of the human body as if they could “touch organs and evaluate their stiffness”, says team member Stephan Catheline of the University of Lyon.
Frequency drop
In the past few years, researchers have developed ways of measuring the shear modulus by using shear waves with a much lower frequency, which propagate further in soft tissue. These waves are created inside the body by firing focused ultrasound through the skin, but this has its drawbacks. The brain, for example, is protected against shock and vibration by both the skull and the thin layer of cerebrospinal fluid lining it, which makes inducing shear waves difficult.
Now Catheline and colleagues have adapted an idea called magneto-acoustical electrical tomography to create the shear waves. This involves passing an alternating electric current through tissue in an applied magnetic field. The resulting electromagnetic Lorentz force induces shear-wave oscillations in the tissue. While other researchers had used a high-frequency alternating current, the team used a frequency of only 10–1000 Hz. Using a synthetic tissue substitute called a phantom, and then a sample of pig liver, the researchers tested out their idea, showing that they could induce low-frequency waves with an electric current and detect them using ultrasound transducers. Their results for the pig liver agreed with accepted values for the shear elasticity of healthy liver tissue.
High electric fields
Before the research can be used in medicine, there are some difficulties to address. First, the researchers needed high electric fields to generate a large enough Lorentz force. They estimate that the electrical current passing through the tissue was 100 times higher than accepted safety limits, albeit only momentarily. However, modern magnetic resonance imaging (MRI) scanners can generate magnetic fields many times higher than the 100 mT available from the permanent magnets in the team’s laboratory: using these, one could generate the same Lorentz force with a lower electric field. Second, the cerebrospinal fluid that prevents ultrasound from getting into the brain would also stop it getting out, so one would need another way to detect cerebral shear waves. Here too, MRI might provide the answer, as it has been used in the clinic to detect tissue oscillations.
Kathy Nightingale, an elastography expert at Duke University in North Carolina, says that “so far, what’s exciting about this research is that it’s the first demonstration that I’m aware of of the generation of shear waves using this Lorentz force approach”. There are clear challenges in liver elastography, her own specialism, on patients with livers further below the skin, such as obese patients, she explains. “If this were to be successful in that population, that could be significant,” she says, but stresses that we will have to “wait and see”.
The research will be published in Physical Review Letters.