Aortic stenosis, the narrowing of the aortic valve, is one of the most common and serious heart valve dysfunctions. Usually caused by a build-up of calcium deposits (or sometimes due to a congenital heart defect), this narrowing restricts blood flow from the left ventricle to the aorta and, in severe cases, can lead to heart failure.
The development of sensitive, cost-effective techniques to identify the condition is paramount, particularly for use in remote areas without access to sophisticated technology. To meet this challenge, researchers from India and Slovenia have created an accurate, easy-to-use and low-cost method to identify heart valve dysfunction using complex network analysis.
“Many rural health centres don’t have the necessary technology for analysing diseases like this,” explains team member M S Swapna from the University of Nova Gorica, in a press statement. “For our technique, we just need a stethoscope and a computer.”
Hear the difference
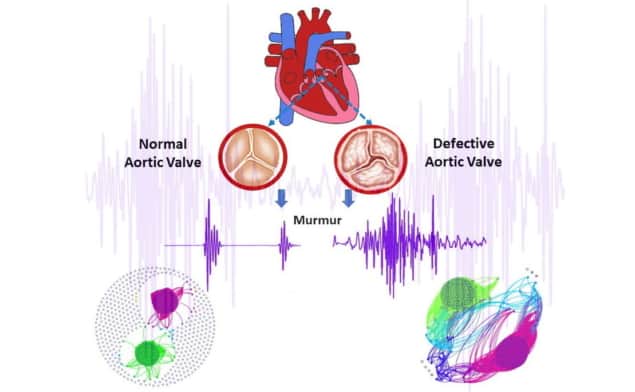
A healthy person produces two heart sounds: the first (“lub”) due to the closing of mitral and tricuspid valves and the second (“dub”) as the aortic and pulmonary valves close, with a pause (the systolic region) in between. These signals contain carry information about the blood flow through the heart, with variations in pitch, intensity, location and timing of the sounds providing essential information related to a patient’s health.
Swapna and colleagues – Vijayan Vijesh, K Satheesh Kumar and S Sankararaman from the University of Kerala – aimed to develop a simple method based on graph theory to identify aortic stenosis heart murmur. To do this, they examined 60 digital heart sound signals from normal hearts (NMH) and hearts with aortic stenosis (ASH). They subjected the signals to fast Fourier transform (FFT), complex network analyses and machine-learning-based classification, reporting their findings in the Journal of Applied Physics.
The researchers first converted each audio signal into a time series. The signal from a representative healthy heart clearly showed the two heart sounds and the separation between them, while signals from hearts with aortic stenosis displayed diamond-shaped murmurs.
Next, the team used FFT to convert the time-domain signals to the frequency domain, thus providing information on the frequency components in the murmur, which vary with valve dysfunction. The FFT analysis for NMH showed well-defined peaks from the two sound signals in a normal heart. For ASH, however, the FFT spectrum contained a large number of signals over a wide frequency range, with no distinct peaks assignable to the lub and dub sounds. These additional components are attributed to vibrations occurring from calcium deposits blocking the aortic valve and creating turbulence in the blood flow.
While both the time-domain and FFT analyses enable preliminary identification of defective valves, to analyse the sound signals further, the researchers used the data to create a graph, or a complex network of connected points. They split the data into sections, with each part represented as a node on the graph. If the sound in that portion of the data was similar to another section, a line is drawn between the two nodes.
In a healthy heart, the graph showed two distinct clusters of points, with many unconnected nodes. The unconnected nodes are likely due to the absence of a time-domain signal in the systolic region, indicating the proper functioning of the heart. The network of a heart with aortic stenosis was far more complex, with two prominent clusters and an absence of uncorrelated nodes, indicative of a potential valve defect.
The team extracted a set of parameters, known as the graph features, from the graph of each signal. These features (the average number of edges, diameter, network density, transitivity and betweenness centrality) can then be used by machine-learning techniques to classify the signals as either ASH or NMH.

Advanced cardiac MRI guides treatment for stiff heart syndrome
Three supervised machine-learning classifiers – K-nearest neighbour (KNN), support vector machine and KNN subspace ensemble – exhibited prediction accuracies of 100%, 95.6% and 90.9%, respectively. This high accuracy suggests that the use of these mathematical concepts could provide greater sensitivity and reliability in digital cardiac auscultation and could be easily employed in rural health centres.
The researchers have so far only tested the method with existing data, not in a clinical setting. They are now developing a mobile application that could be accessed worldwide. “Currently, we are analysing other heart murmurs to make a comprehensive analysis of heart murmurs,” Swapna tells Physics World. “After that, the work will be extended to real-world data by directly recording the sound with the help of a medical practitioner. The development of software and a mobile application comes in the third stage of work.”



