Stereotactic ablative radiotherapy (SABR) is a standard-of-care treatment for patients with early-stage thoracic tumours, and can be safely and effectively delivered in a single fraction. The Amsterdam University Medical Centers (VUmc) implemented MR-guided SABR in 2016, immediately applying the technique to treat thoracic tumours. The researchers have now demonstrated that it’s possible for patients to receive MR-guided SABR for lung cancer – including consultation, treatment simulation and planning, and radiation delivery – in a single day.
Previous studies have shown that single-fraction SABR for lung tumours is equivalent to fractionated SABR in terms of local control, progression-free survival, overall survival and toxicity. Adding MR-guidance brings additional benefits: online planning tailored according to the patient’s anatomy of the day; real-time imaging of the tumour position; and gated delivery. MR-guided radiotherapy improves upon conventional image-guided radiotherapy by providing high soft-tissue definition without any additional radiation exposure.

Led by Miguel Palacios and Suresh Senan, clinicians in the department of radiation oncology conducted a 10-patient study to investigate the clinical feasibility of delivering MR-guided SABR for early-stage lung tumours in a single day – referred to as a “one-stop-shop”. The researchers report their successful experience in Physics and Imaging in Radiation Oncology.
The study included 10 patients aged 63 to 85 years. All had small lung tumours (no larger than 5 cm in diameter), with gross tumour volumes (GTVs) ranging from 1.3 to 22.9 cm3 (median 2.2 cm3). The prescribed doses for these patients ranged from 28 to 34 Gy.
Prior to their appointment, patients had a telephone conversation with a radiation oncologist, who explained the procedure and also determined that the patient was fit enough to have everything done in a single day.
On the day, the one-stop-shop treatment started with a 20 min in-person consultation with the radiation oncologist. The patient then underwent MR simulation using the MRIdian MR-guided radiotherapy system, which included at least one 3D MR scan in shallow inspiration/expiration breath-hold. Next, the team performed MR-cine scans in the sagittal, coronal and axial planes to determine tumour motion characteristics.
During the MR simulation, patients were given repeated breath-hold instructions to determine their ability to understand and comply with breath-hold procedures. To assist patients during breath-holds, real-time MR-cine frames showing the GTV and tracking boundary contours were displayed on an MR-compatible monitor. This also enabled patients to gain confidence in the video-assisted delivery procedure.
The choice between gating in inspiration or expiration breath-holds was made on the basis of patient convenience and compliance, as well as a visual assessment of the automatic tumour contour “tracking”. Ultimately, nine patients were treated in inspiration breath-hold and one in expiration breath-hold.
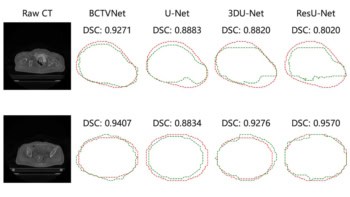
After the MR simulation, the researchers imported the 3D MR into the MRIdian treatment planning system (TPS) for delineation of the target and organs-at-risk (OARs). A CT scan performed in the selected breath-hold state was also imported into the TPS, enabling the physician to compare the MRI-based GTV contour with the CT-based contour and make adjustments at their discretion.
The researchers used the TPS to generate treatment plans for step-and-shoot intensity-modulated radiotherapy. A planning target volume (PTV) margin of 5 mm around the GTV and a 3 mm gating boundary were generated to account for intra-fraction residual motion and possible microscopic tumour spread. They explain that this approach led to an overall improvement of the GTV area covered during beam-on, with an average of at least 94.4% of the GTV always present inside the PTV.
The MR-guided SABR treatments were delivered with real-time visual feedback of the actual GTV position. Radiotherapy was performed in two consecutive sessions, with a rest period between each. This protocol minimized fatigue by elderly patients caused from repeated breath-holding, and limited the time during which patients had to lie completely still.

MRI guidance minimizes toxicity in prostate cancer radiotherapy
All 10 patients successfully completed the one-stop-shop treatment, with the entire procedure, including waiting time, taking less than 7 h. Median durations were 0.3 h for consultation, 1.1 h for simulation, 2.8 h for planning, review and approval, and 1.2 h for delivery. The researchers note that they were able to reduce the time required for treatment planning by employing semi-automatic contouring of sensitive structures around the target and performing pre-treatment planning on a previous diagnostic CT scan. This shorter duration resulted in higher patient satisfaction survey scores – assessed via patient questionnaires following treatment completion.
“We are adding new functionality to our MR-linac which will improve our single-day SABR planning and treatment delivery,” Palacios tells Physics World. “We will extend this procedure in the next months after refinement of our procedure. Taking into account the high patient satisfaction, we intend to offer the one-stop-shop service to patients with tumours in the abdomen, such as adrenal gland metastases.”