Researchers at the Mayo Clinic have combined photon-counting detector (PCD) CT with deep learning-based noise reduction to image patients with multiple myeloma. The new imaging technique demonstrated superior detection of bone disease associated with multiple myeloma compared with conventional low-dose, whole-body CT scans.
PCD CT works by directly converting individual X-ray photons into an electric signal. This allows the use of smaller detector pixels, thereby increasing the image spatial resolution and improving detection of lytic lesions – areas of bone destruction found in around 80% of multiple myeloma patients. This improvement could make a difference in the staging of disease, and potentially impact therapy choice and patient outcomes.
Multiple myeloma is a cancer of plasma cells, a type of white blood cell. Cancerous myeloma cells grow out of control, crowding out normal plasma cells and preventing them from making antibodies to fight infection. Patients may initially be asymptomatic, or develop smouldering multiple myeloma, an intermediary disease phase characterized by a significant increase in plasma cell proliferation, but without any organ damage or symptoms. Active multiple myeloma can cause a range of symptoms, including bone pain, hypercalcaemia, renal insufficiency, anaemia and/or lytic bone lesions.
“When a single lytic lesion larger than 5 mm can be seen on CT, this is a myeloma-defining event that will upstage a patient to active status and require a conversation about initiating treatment,” says principal investigator Francis Baffour.

“Patients suspected of having multiple myeloma undergo a battery of tests, including bone marrow biopsy. But random biopsy sampling from just one location may not detect the true burden of the disease,” Baffour explains. “Because of its high sensitivity and specificity for lytic bone lesions throughout the body, the International Myeloma Working Group recommends low-dose, whole-body CT as the imaging test to evaluate lytic bone lesions.”
Baffour and colleagues sought to prove that PCD CT, combined with the deep learning denoising software developed by the Mayo team, would increase spatial resolution enough to improve diagnosis using the same radiation dose as a conventional energy-integrating detector (EID) CT scan.
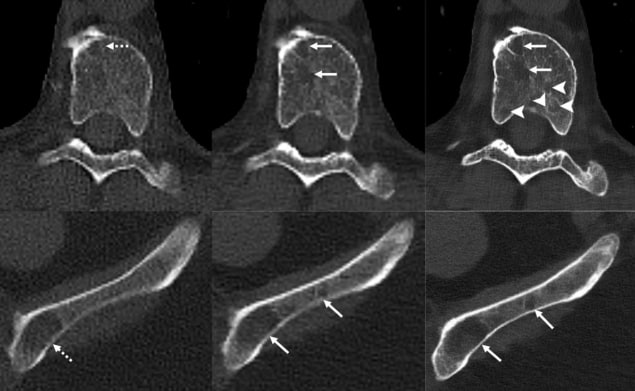
The study, reported in Radiology, included 27 adult patients with different stages of multiple myeloma. Participants underwent both types of scan on the same day: a low-dose, whole-body EID CT scan; and a PCD CT scan at a matched radiation dose (8 mSv for an average adult). The researchers reconstructed EID CT and PCD CT images at 2 mm section thickness. They also reconstructed thinner 0.6 mm PCD CT image sections, which were denoised using a convolutional neural network.
To compare the corresponding 2 mm images, two musculoskeletal radiologists blinded to patient demographics, CT scanner type and scan protocols independently scored the images for features that determined myeloma activity. These included: lytic lesions in the skeleton; hyperdense nodular soft-tissue lesions in the medullary cavity; fat attenuation in myeloma lesions; and pathologic fractures.
The researchers report that PCD CT exhibited superior performance across all visualization assessments, with the strongest differences observed for viewing lytic bone lesions, intramedullary lesions and fat attenuation.
Four weeks later, the radiologists compared the denoised 0.6 mm PCD CT images with the 2.0 mm EID CT images. For each patient, they also recorded the change in the number of detected lytic lesions from the previous set of images. The thin-section PCD CT images again demonstrated improved viewing of all four pathologic abnormalities. Additionally, the readers observed a higher number of lytic lesions on PCD CT relative to EID CT images in 21 of the 27 participants.
“An increase in the number of lytic lesions is highly suggestive of disease progression,” explains Baffour. “When a patient progresses, therapy may be initiated if the patient was previously not being treated or changed if the patient was on therapy. Lytic lesions weaken the bone and, in some locations, put the patient at risk of developing fractures.”
Baffour points out that the improved spatial resolution of PCD CT allows visualization of small structures and more detailed features that may suggest that a lesion is healing or has been treated. “For example, if we see that a lesion has developed a sclerotic rim or has new internal fat density when there was soft tissue previously, we know that the patient has undergone treatment,” he explains.

Photon-counting CT promises a new era of medical imaging
Baffour tells Physics World that he and his colleagues would like to observe a cohort of patients in various multiple myeloma precursor states, to determine the frequency of new lytic lesions. They also want to investigate PCD CT in other instances in which low-dose protocols are beneficial, such as for paediatric or pregnant patients or screening applications.
“Here at Mayo Clinic, studies are underway to determine how low we can go with scanning doses while still obtaining diagnostic CT images,” says Baffour. “There is much on the horizon and so much potential for photon-counting detector CT in clinical care.”