Monitoring and controlling the radiation delivered to every patient is of utmost importance in radiation therapy. This is a current challenge in emerging ultrahigh-dose rate modalities such as electron FLASH (eFLASH) radiation therapy.
FLASH radiotherapy delivers radiation at ultrahigh dose rates, shortening the treatment course and improving tissue sparing relative to conventional radiotherapy.
“One of the things that we need to elucidate [with FLASH] is what is the biological mechanism behind the sparing effect and how does it depend on the way that we are delivering these ultrahigh dose rates. To determine that we need to know exactly what we’re delivering,” explains Emil Schüler from the University of Texas MD Anderson Cancer Center. “Having a good understanding of the exact parameters for each pulse that is being delivered seems to be important. Until we know more, we need to have that type of detailed understanding of our deliveries, and that is where conventional equipment has proved to be suboptimal.”
In conventional radiotherapy, radiation delivery is monitored using transmission ion chambers. While ion pairs occasionally recombine in these dosimeters, ion recombination represents only a small percentage of measurements (less than 5%) and these events can be accounted for using models and correction factors. In high-dose rate eFLASH beams, however, over 90% of ion pairs might recombine, conventional models that correct for ion pair recombination break down, and accurate beam monitoring and control becomes challenging – if not impossible.
Led by Schüler and Sam Beddar, a team of MD Anderson researchers has recently described a way to overcome the challenges inherent to eFLASH beam monitoring. Their solution has its roots in high-energy physics experiments.
Beam current transformers for FLASH
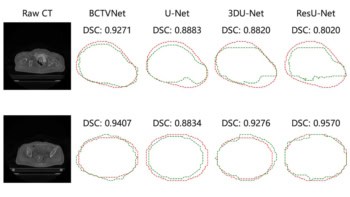
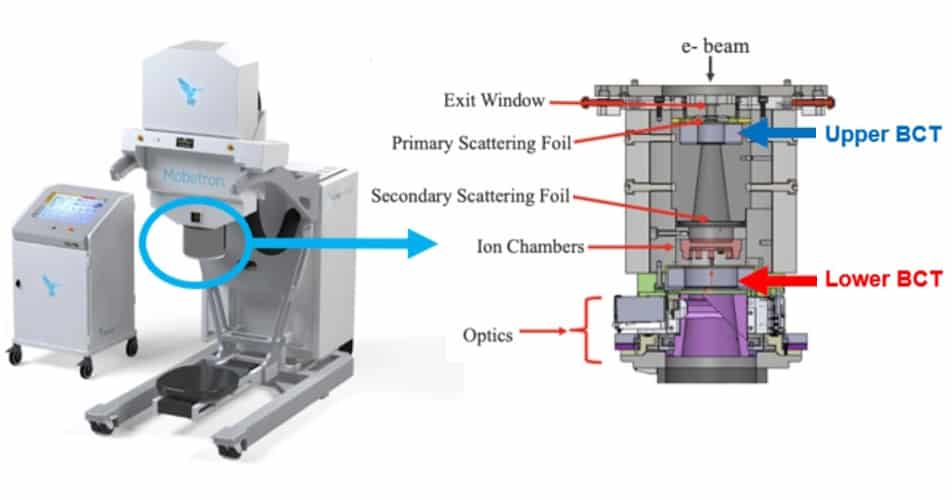
In their study, reported in the Journal of Applied Clinical Medical Physics, the researchers introduce an integrated beam current transformers (BCTs) system to monitor radiation beams produced by the Mobetron system, a commercial electron therapy linear accelerator manufactured by IntraOp.
BCTs, which were originally used in the beamlines of high-energy physics experiments, measure the induced current of electrons passing through them. Building on work performed at Lausanne University, IntraOp engineers redesigned the Mobetron head to accommodate two BCTs: one located after the primary scattering foil; the other, downstream of the secondary scattering foil.
The MD Anderson researchers then extensively characterized the BCT response to ultrahigh-dose rate electron beams at 6 and 9 MeV. They monitored beam output in different dosimetric setups and with different collimation as a function of dose, scattering conditions, and physical beam parameters including pulse width, pulse repetition frequency and dose per pulse. Dosimetric evaluations were performed with GafChromic EBT3 film, a standard dosimeter that gives total dose readings independent of dose rate. Experimental studies were performed three times to ensure repeatability and reproducibility.
The team concluded that BCTs can accurately monitor eFLASH beams, quantify accelerator performance and capture essential physical beam parameters on a pulse-by-pulse basis.
Now, they are investigating the source of, and ways to correct for, higher differential backscatter levels measured in the upper BCT relative to the lower BCT. These discrepancies were measured outside the range of likely clinical eFLASH beam parameters. Schüler and Beddar’s team is also developing methods to measure beam flatness and symmetry, which to date cannot be measured with BCTs.

Photons, protons or electrons: which will bring FLASH radiotherapy to the clinic?
The overarching goal of this research, Schüler says, is to make sure that radiation physicists can deliver eFLASH radiation treatments accurately and precisely.
“It really comes down to making sure that we can guarantee a safe and robust clinical translation of this technology,” Schüler says. “For medical physicists, this is going a little bit outside of our comfort zone…going outside of the standard equipment that we are using now, when FLASH radiotherapy is becoming a reality. We also trying to develop the ion chamber technology for these ultrahigh dose rates, but for [beam] monitoring, especially when it comes to electron beamlines, it’s unlikely that we’re going to be able to use transmission chambers in the same fashion as we have previously with conventional dose rate radiotherapy.”