Alzheimer’s disease is a neurodegenerative disorder with limited treatment options. The causes of Alzheimer’s are complex and not entirely understood. It is commonly thought, however, that the build-up of amyloid-beta plaques and tangles of tau proteins in the brain leads to nerve cell death and dementia. A team at the University of Utah is investigating a new way to use radiation to reduce such deposits and potentially alleviate Alzheimer’s symptoms.
Developing a therapy for Alzheimer’s disease is a key goal for many researchers. One recent study, for example, showed evidence that reducing amyloid-beta plaques with a newly approved antibody-based drug improved cognition in patients with early-stage Alzheimer’s. Alongside, scientists are studying non-pharmacological approaches such as whole-brain, low-dose ionizing radiation, which has been shown to break up plaques in mice and exhibited a positive cognitive effect in preliminary clinical studies.
While promising, whole-brain irradiation unavoidably delivers radiation dose to healthy tissues. Instead, the University of Utah team is exploring the potential of targeted alpha therapy (TAT) to reduce amyloid plaque concentrations while minimizing damage to healthy tissue and the associated side effects.
“Our goal was to build on these studies and, as opposed to irradiating the whole brain, target the plaques specifically,” explains lead author Tara Mastren. “TAT could have potential benefits compared to the current antibody treatment, as much smaller doses are required to achieve an effect. Currently, it is hard to say if it will be better as this is new territory and studies need to be done to prove that.”
Targeted irradiation
TAT works by delivering an alpha particle-emitting radionuclide directly to a target, where it releases energy into its immediate surroundings. As alpha particles only travel a few micrometres in tissue, they deliver a highly localized dose. The approach has already proved effective for treating metastatic cancers, and the Utah team postulated that it could also be used to break bonds within amyloid-beta aggregates and facilitate plaque clearance.
To perform TAT, Mastren and colleagues synthesized a compound called BPy (a benzofuran pyridyl derivative) that targets amyloid-beta plaques. They linked BPy to the radionuclide bismuth-213 (213Bi), which has a short half-life of 46 min and decays by emitting a single alpha particle, thereby creating [213Bi]-BiBPy.
To examine whether TAT could reduce amyloid-beta concentrations, the researchers incubated [213Bi]-BiBPy with homogenates created from the brain tissue of mice genetically modified to develop amyloid plaques. After 24 h, they measured the concentration of amyloid-beta in the samples using Western blot and enzyme-linked immunosorbent assays.
Both analysis methods revealed a significant, dose-dependent reduction in amyloid-beta following incubation with [213Bi]-BiBPy, with plaque reduced to below the detection limits. Incubating the brain homogenate with free 213Bi also reduced levels of amyloid-beta, but to a significantly lesser extent. Other proteins in the homogenate were not affected, suggesting a lack of off-target damage.
The team found that a dose of 0.01488 MBq per picogram of amyloid beta was required to reduce amyloid by 50% in vitro. Mastren notes that this finding must now be investigated in vivo, as biological processes in a living brain differ from those in postmortem tissue. “However, this value gives a starting point for our in vivo studies,” she adds.
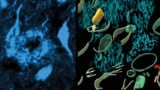
To confirm the targeted binding of [213Bi]-BiBPy, the researchers also examined 10 µm-thick brain tissue sections from the mice. They stained the sections with a fluorescent BPy probe (fluorescein-functionalized) and with thioflavin-S, an amyloid stain. Thioflavin-S revealed a dense presence of plaques, particularly in the cortex. The fluorescent BPy probe also stained plaques in the cortex, but less intensely and with more off-site binding. This finding highlights the need to investigate alternative targeting vectors to reduce white-matter binding.
Cryo-electron tomography reveals structure of Alzheimer’s plaques and tangles in the brain
The researchers conclude that TAT can significantly reduce amyloid-beta aggregates in vitro, paving the way for studies in live animals and eventually in humans. As such, they plan to start in vivo testing of TAT later this year.
“Initially, we will be looking at the biodistribution, ability to cross the blood–brain barrier, immune response to treatment and effects on plaque concentrations,” says Mastren. “If successful, we hope to follow up with testing cognitive response to treatment.”
The research is described in the Journal of Nuclear Medicine.