Deep learning-based contouring of multiple brain metastases eases clinical workload when planning stereotactic radiosurgery treatments
Brain metastases – cancerous lesions that have spread from elsewhere in the body – are increasingly treated using stereotactic radiotherapy (SRS), a precision technique that targets each individual lesion with a high dose of radiation. Compared with whole-brain irradiation, SRS may lead to higher local control and increased cognitive sparing, as well as a shorter overall treatment duration. But to target and treat multiple brain metastases, each lesion must first be detected on an MRI scan and accurately delineated. And this can be a complex and time-consuming task.
“There are two challenges that we face in the clinic,” explains Evrim Tezcanli, professor of radiation oncology at Acibadem Atasehir Hospital in Turkey. “First, we want to treat all the lesions. But very small lesions, particularly those under 0.1 cc, can easily be missed by untrained eyes. Larger metastases, meanwhile, are more challenging to contour – you want to cover the whole lesion without missing a pixel, but don’t want to spill radiation over into the brain tissue. It’s time-consuming work, especially if there are multiple lesions.”
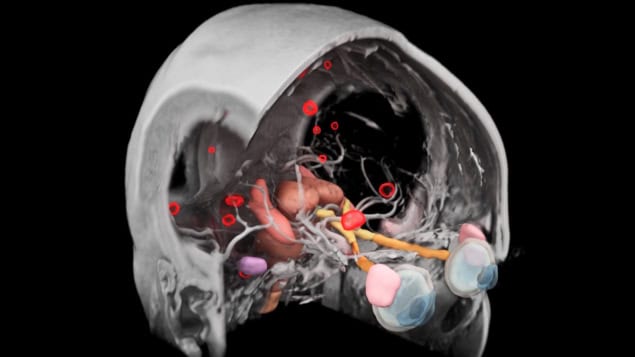
To address these challenges, Siemens Healthineers has developed an AI-powered software tool that automates the contouring of brain metastases. The software – integrated into the company’s syngo.via RT Image Suite and AI-Rad Companion Organs RT packages – employs advanced deep-learning algorithms to rapidly analyse a patient’s MR images and contour and label metastatic lesions. Alongside, it delineates key organs at risk, such as the brainstem and optic structures.
“One of the main strengths of this software is that it reduces the manual workloads really well,” says Tezcanli.
Meeting clinical standards
To evaluate the accuracy and time efficiency of the new software tool, Tezcanli and her team compared AI-based delineation with the performance of two experienced radiation oncologists. The study included data from 10 patients with between three and 17 brain metastases. The radiation oncologists manually contoured all lesions (82 in total) based on patients’ contrast-enhanced MRI scans; the same images were also processed by the AI software to automatically contour the metastases.
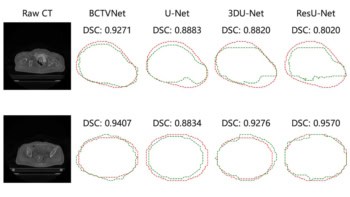
Tezcanli reports that the software performed remarkably well. “One of the most significant findings was that the manual contours and the AI-generated contours showed strong agreement, especially for lesions larger than 0.1 cc. In terms of geometric similarity, the AI-generated boundaries were well within our clinically acceptable levels,” she says.
Comparing the manual and AI-generated contours revealed a medium Dice similarity coefficient of 0.83, increasing to 0.91 when excluding very small lesions, and a median Hausdorff distance (the maximum distance between the two contours) of 0.3 mm.
AI will definitely have a place because of the time savings and accuracy it delivers
Evrim Tezcanli
To quantify the overall time efficiency, the researchers timed the contouring process for the radiation oncologists and the AI tool. They also measured the time taken for expert review of the AI-generated results, in which a radiation oncologist checks the contours and performs any necessary adjustments before they are approved for treatment planning.
The AI software completed the contouring for each patient in just one to two minutes, reducing the workload by an average of 75%, and in some cases saving over 30 minutes per patient. “We still needed to review the AI contours, but the correction time was only three to four minutes,” says Tezcanli, emphasizing that expert review remains essential when using AI. “One case required nine minutes, but even with that patient we had a time saving of 75%.”
As well as saving time for the oncology staff, AI-based contouring has a lot to offer from the patient’s perspective. Spending less time on demanding manual contouring frees up the physician to spend more time with the patient.
Lesion detection
For their study, the researchers analysed post-contrast T1 MPRAGE sequences recorded using a 3 Tesla MRI scanner. To maximize lesion enhancement, they acquired images several minutes after contrast injection, though Tezcanli notes that this timing may vary between treatment centres. They also used image slices of 1 mm or less. “This is a very precise treatment and we want to make sure everything is accurate,” she adds.
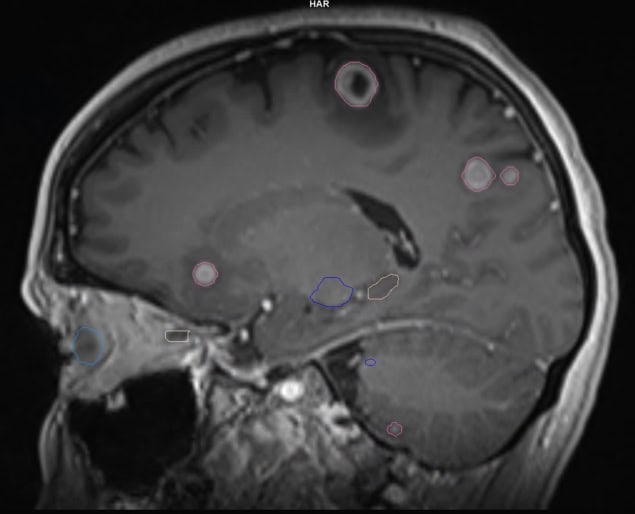
The study deliberately included patients with varying numbers of different sized metastases, to assess the algorithms under diverse clinical scenarios. In terms of lesion detection, the software exhibited an overall sensitivity of 94% – finding 77 of the 82 metastases. The five missed lesions were extremely small, 0.01 to 0.03 cc, a volume that’s challenging even for physicians to detect. The software did, however, find three additional lesions that were not originally identified and which were later confirmed as brain metastases.
The false positive rate was 8.5%, with the software mistakenly identifying seven vascular structures as metastases. “Because the algorithms work with contrast enhancement, any vascular enhancements that mimic the tumour can be mistaken,” says Tezcanli. “Here we needed to use a dedicated MRI sequence to define whether it was a metastasis or not. That’s just one thing to be cautious about. Other than that, we were very satisfied with the software’s ability to detect small lesions and find ones that we hadn’t detected.”
Automation with HyperArc
The contours generated by the AI software are exported in DICOM RT Struct format, enabling direct transfer into the treatment planning system. At Acibadem Atasehir Hospital, this next step is performed using HyperArc, a radiosurgery-specific software module within the Eclipse treatment planning infrastructure. HyperArc performs automated treatment planning and delivery, enabling fast and efficient SRS on the Varian TrueBeam and Edge linacs.
“HyperArc has proven to be highly effective, even when treating patients with multiple brain metastases,” says Burcin Ispir, a medical physicist working alongside Tezcanli. “One of its biggest powers is its ability to perform single isocentre, automated planning for multiple targets, which significantly reduces planning time while maintaining excellent plan quality. In our experience, HyperArc-generated plans offer high conformity and steep dose gradients, which are critical for sparing normal brain tissue.”
Unlike conventional radiotherapy where homogeneity is desirable, SRS plans intentionally allow controlled heterogeneity within the target volume to improve sparing of normal tissue. HyperArc also offers automation of the beam geometry, including collimator and couch angles, ensuring consistent, fast and highly reproducible plans “For selected cases, we have found this enables a same-day workflow where contouring, planning and treatment can all be completed within a single day,” Ispir explains.
Intelligent solutions streamline radiotherapy treatment planning
The automation in AI contouring and HyperArc planning speeds up the treatment planning process, and when compared to traditional workflows, potentially allows patients to commence radiation therapy treatments earlier. The ability to commence treatment as soon as possible after the MRI scan is imperative when treating brain metastases. Most patients will also be receiving systemic therapies, which need to be delivered on schedule. But perhaps more importantly, the high spatial precision of SRS makes the technique sensitive to even small anatomical changes within lesions. If the delay between MR imaging and radiotherapy treatment is too long, any changes occurring during that time could decrease targeting accuracy.
“We are in an era where we are using the technology to have even same-day treatments,” says Tezcanli. “We have rapid contouring with AI, a quick review of a few minutes by the expert radiation oncologist, treatment planning with HyperArc, and then a few hours later the patient is treated. This is where the technology is taking us.”
Look to the future
Continuing improvements in cancer treatment techniques mean that patients are living longer, but this also increases the likelihood of metastases developing. In addition, higher quality MRI scans and enhanced imaging protocols lead to more metastases being detected. These factors combine to increase the workload on centres treating multiple metastases with SRS.
“I think we will be treating brain metastasis more and more,” says Tezcanli. “And I think radiosurgery will be the main treatment modality in the future. AI will definitely have a place because of the time savings and accuracy it delivers. And this is only the first version of the software; I’m sure it can be improved to find even smaller lesions or differentiate vascular structures.”
Following the initial software evaluation, the team has not yet fully integrated it into their clinical routine, but Tezcanli tells Physics World that they would be happy to use the software in every one of their brain metastases treatments. “I think we will be using it routinely in the future in all of our clinical cases,” she says.
-
The statements by customers of Siemens Healthineers described herein are based on results that were achieved in the customer’s unique setting. Because there is no “typical” hospital or laboratory and many variables exist (e.g., hospital size, samples mix, case mix, level of IT and/or automation adoption) there can be no guarantee that other customers will achieve the same results.
The products/features mentioned herein are not commercially available in all countries. Their future availability cannot be guaranteed.
Autocontouring results are generated by Siemens. The displayed renderings are created with software that is not commercially available.