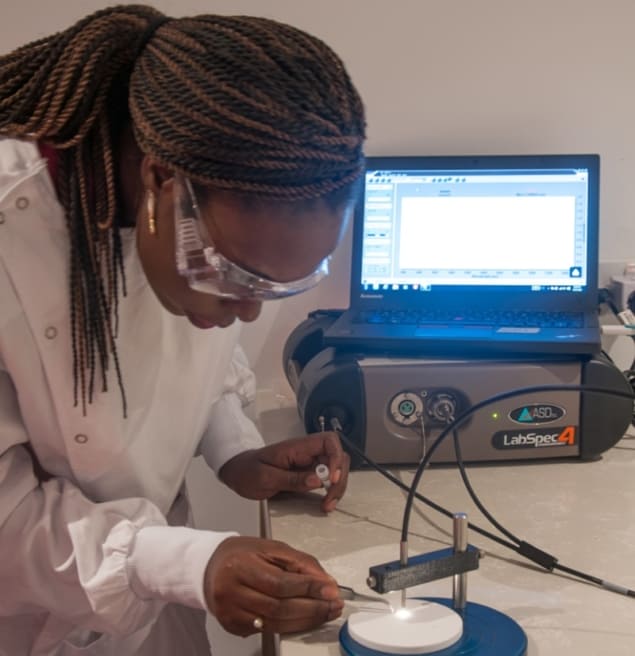
Zika virus can now be detected inside mosquitoes 18 times faster and 110 times cheaper than before – by shining light on them. Researchers have used near-infrared spectroscopy (NIRS) to detect Zika virus in laboratory mosquitoes for the first time (Science Advances 10.1126/sciadv.aat0496). The team, led by Maggy Sikulu-Lord from the University of Queensland, working with colleagues from Brazil and the USA, tested NIRS as an alternative to the current approach: reverse-transcription polymerase chain reaction (RT-qPCR).
NIRS generates different spectra based on the chemical composition of the mosquito. While it is not understood which chemicals are responsible for the difference in spectra between infected and uninfected mosquitoes, the spectra are different enough to distinguish the two with more than 90% accuracy seven days after infection.
Why screen mosquitoes?
Zika virus became a major health concern in 2015 when an epidemic in Brazil was linked to microcephaly, a condition where babies are born with small heads. The virus can also cause Guillain-Barre syndrome, a neurological disorder, in adults. Female Aedes aegyptis mosquitoes transmit the Zika virus, but a study from 2016 found that only 0.9% of these mosquitoes carry the virus. To identify the infected mosquitoes, rather than wasting containment efforts on the over 99% of uninfected mosquitoes, called for a quick, simple and cheap screening method.
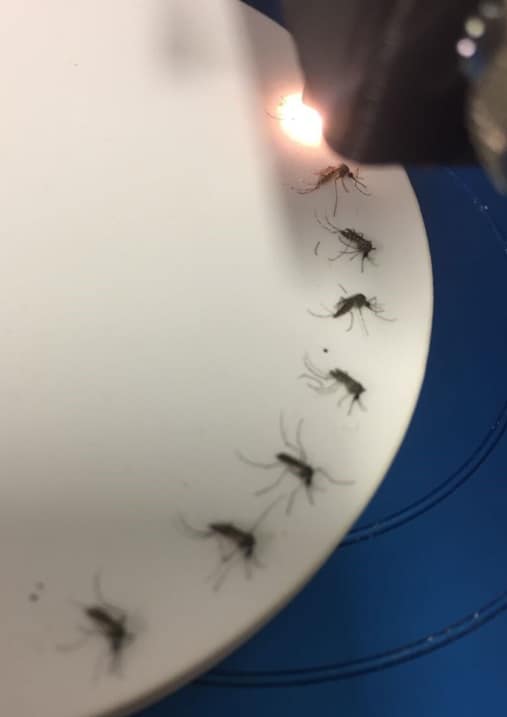
The low rate of infected mosquitoes means that an efficient screening programme would need to screen thousands of mosquitoes in a day. RT-qPCR is too slow and too expensive to work on such a large scale, first author Jill Fernandez and her team argue. NIRS, on the other hand, does not need sample preparation and therefore lends itself to high throughput screening that can be performed by non-expert staff.
The researchers fed half of their mosquitoes blood infected with Zika virus and the other half with uninfected blood. After four, seven and 10 days, they used NIRS to analyse the head, abdomen and thorax. While head and thorax samples provided the most accurate distinction between infected and uninfected mosquitoes, abdomen samples still gave at least 80% accurate predictions and can be used when head and thorax are not available.
Getting NIRS “field ready”
The results suggest that NIRS might be a suitable screening tool for Zika virus in mosquitoes. However, several questions need to be answered before NIRS is “field ready”, as the authors point out. The method needs to be tested on mosquitoes caught in the wild, rather than ones bred in a laboratory, because there is more variation among wild mosquitoes and because they may be damaged. Further, it needs to be tested whether the method can distinguish different types of viruses inside the mosquito. After all, Aedes aegyptis mosquitoes can not only be infected with Zika but also with other viruses such as Dengue, which causes Dengue fever.
One limitation of NIRS is the initial price. Sensitive NIR spectrometers currently cost $60,000, an investment that is made good after screening 10 000 mosquitoes. Whether less sensitive spectrometers, which are available for less than $500, could distinguish the mosquitoes equally well remains to be investigated. The authors hope that a demand for cheap and sensitive NIR spectrometers will bring the price down and that further savings can be made by increased speed as staff become familiar with the instrument and method.
NIRS has been used for various applications in agriculture and medicine for decades, but only in the last ten years was its value in the field of infectious diseases discovered. This is the first time that NIRS has been used to detect pathogens in mosquitoes. Should it turn out to be a useful tool to detect Zika in the field, other mosquito-transmitted diseases might benefit from the development too.