Proton therapy offers improved spatial dose delivery compared with photon- or electron-based radiotherapy. Meanwhile, recent studies suggest that FLASH radiotherapy – in which radiation is delivered at ultrahigh dose rates – can decrease normal tissue damage while maintaining anti-tumour activity. Combining the two could offer the intriguing possibility of enhancing proton therapy’s intrinsic spatial advantages with the unique temporal effects of FLASH.
With this goal, a team at the University of Pennsylvania has designed a novel treatment system that delivers FLASH proton therapy (FLASH-PRT) using double-scattered protons under CT guidance. In studies on mice, the researchers also report the first demonstration of FLASH-PRT-mediated normal tissue radioprotection (Int. J. Radiat. Oncol. Biol. Phys. 10.1016/j.ijrobp.2019.10.049).
Adapting the output
Using the ProteusPLUS accelerator employed for clinical treatments at the Roberts Proton Therapy Center, the team designed and constructed an apparatus that can deliver protons at either FLASH (60–100 Gy/s) or standard (0.5–1 Gy/s) dose rates.
“We worked extensively with the IBA engineers to achieve robust delivery for these extremely high dose rates,” explains co-senior author Keith Cengel. “This mostly involved tuning of the beamline and developing a control system to request/start/stop beam delivery.”
Cengel notes that the ability to adapt a commercial proton therapy system for FLASH depends on the type of accelerator, as well as beamline characteristics and nozzle type. He suggests that it may be easier to adapt for proton FLASH in a multi-room cyclotron-based facility.
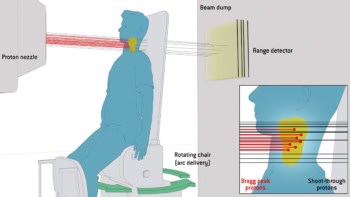
The researchers used the single pencil beam delivered into the centre’s dedicated research room to create a double-scattering system with a uniform and expanded field size (thus removing the additional variable of spot-scanning speed). The apparatus controls dose rate using the proton beam current, with all other system elements identical, thereby ensuring that dose rate is the only difference between FLASH and standard conditions.
The team also developed dedicated dosimetry tools, an essential requirement for FLASH studies. “We built and tested a double-scattering apparatus with real-time verification of absolute dose rate and time–dose structure and ensured that this system was capable of accurately measuring and delivering the desired target dose within typical clinical tolerances,” says Cengel.
Depth–dose profiles of the both FLASH and standard proton beams demonstrated that the entrance region had relatively homogeneous dosimetry. The researchers also confirmed that dose rate in the entrance portion of the beam was linear with beam current, up to 300 nA. Measuring the 3D uniformity of the collimated beam using EBT3 film in solid water phantoms, for the 1 x 2 cm collimator used in animal studies, revealed that 100% of the target was covered by 90–95% of the desired dose.
In vivo advantages
Cengel and colleagues performed in vivo studies to compare the impact of dose rate on normal tissue damage and tumour growth. During irradiations, they used a NaI(TI) crystal detector to measure prompt gamma rays emitted at the beam line exit window and obtain the real-time delivered dose rate.
For the first study, they randomly assigned mice to receive 15 Gy whole-abdominal irradiation using either FLASH-PRT (78±9 Gy/s) or standard proton therapy (0.9±0.08 Gy/s). FLASH significantly reduced the loss of proliferating cells in intestinal crypts (required for self-renewal of the epithelium) compared with standard dose rate treatment, although both approaches decreased numbers compared with nonirradiated controls.
The researchers also evaluated long-term effects in mice exposed to 18 Gy focal intestinal irradiation. Eight weeks after treatment, they observed pronounced fibrosis on intestines irradiated using standard proton therapy. Such intestinal injury is a common side effect for patients with gastrointestinal tumours treated using focal radiotherapy, and can limit the deliverable dose. In contrast, FLASH-irradiated animals experienced significantly less fibrosis, with intestines qualitatively resembling nonirradiated tissues.
Finally, the team treated mice bearing pancreatic flank tumours with a dose of 12 or 18 Gy, using FLASH or standard proton therapy. The target encompassed the tumour and the upper intestine. Both approaches showed a similar dose-dependent inhibition of tumour growth, essentially translating to an increased therapeutic window for FLASH-PRT.

Small-animal irradiation platform performs preclinical proton studies
The team is now working to simultaneously improve the system, define the physical parameters of biological outcome (time–dose–fractionation, for example) and better understand the fundamental mechanisms by which FLASH retains tumour effect while sparing normal tissues.
As for when FLASH-PRT may possibly be ready to enter clinical trials, Cengel says that this will depend on the outcome of upcoming studies. “The time before human clinical trials is likely to be measured more in years than in months,” he tells Physics World. “But we are particularly excited about the possibility of starting clinical trials in veterinary oncology patients.”