A US-based research team has successfully demonstrated how dynamic stimulation of the visual cortex enables blind and sighted people to “see” shapes – a technique that could one day be used to convey entire visual scenes to patients.
Neuroscientists and neurosurgeons have long known that electrical stimulation of electrodes implanted in the visual cortex using small currents produces the perception of a small flash of light, known as a phosphene. This process could serve as the basis for a visual cortical prosthesis (VCP), a device that could restore some visual abilities to blind patients. Although some VCPs were tested in the 1960s and 1970s, they had limited effectiveness and were constrained by the technology of the time. But now a new wave of teams are attempting to produce a modern VCP, using improved electrodes and better wireless data and power transfer technology.
Two such teams, based at Baylor College of Medicine (BCM) and the University of California, Los Angeles (UCLA), have carried out clinical trials and tests of a VCP device called Orion, produced by Second Sight Medical Products. The results, recently published in the journal Cell, show that the Orion device is a safe and effective means of providing patients with some visual experience.
“Our research team is specifically trying to understand how to make the subjects be able to see and discriminate between visual forms such as simple objects or letters. Our key finding is that we can more effectively communicate visual forms to the subject if we use a dynamic electrical stimulation protocol,” says William Bosking, assistant professor of neurosurgery at BCM, who co-wrote the article with senior author Daniel Yoshor, professor of neurosurgery at BCM.
Put simply, this means that instead of treating the electrodes on the array like pixels in a video display, and sending various current levels to all of them at once in an attempt to convey a particular form or shape to the patient, the device instead stimulates only the electrodes that outline the shape it is trying to convey, and stimulates them in a rapid dynamic sequence.
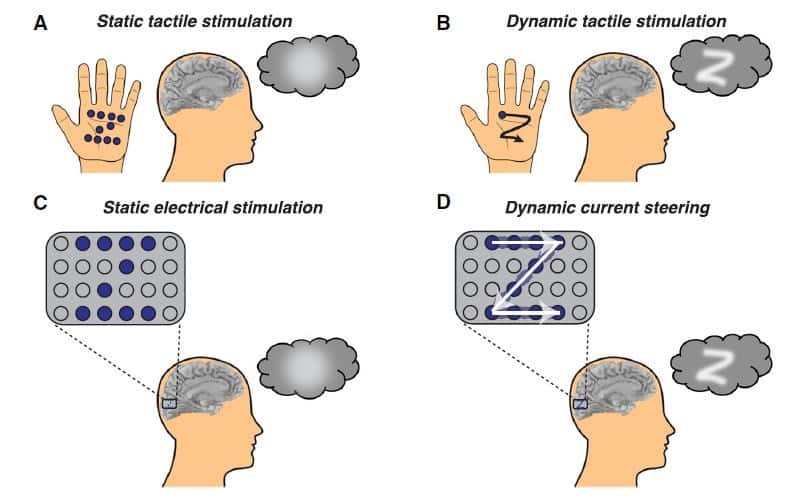
“This is analogous to how you might trace out a letter on someone’s palm or forearm if you were trying to convey a letter to them by touch,” explains Bosking. “We find that using this dynamic sweeping of activity across the visual cortex allows the subjects to perceive and discriminate letters reliably.”
Visual scenes
The Orion VCP system consists of a camera, which captures an image of the visual scene in front of the patient, a visual processing unit that the subject wears on their belt and which performs some filtering of the camera image, and a transmitter worn on a headset that delivers wireless data and power to a receiving coil implanted under the skin. It also contains circuitry to handle the final conversion of signals into currents to be sent to the electrodes, as well as the electrode array itself, which consists of a flexible sheet with 60 embedded electrodes that lies on the surface of the visual cortex.
“Our research team focuses on understanding how to use the implanted electrodes to produce the best visual experience for the patients. Second Sight is the hardware manufacturer in this case, and we are trying to understand how to best use that hardware to allow the patients to see and discriminate visual forms,” says Bosking.
Bosking notes that with VCPs tested in the past, subjects did not really see or perceive coherent visual forms, instead they tended to see blobs of light in front of them in various locations. “Our new electrical stimulation protocol … produces more coherent perception of visual form, and sends less current to the brain,” he adds.
Looking ahead, the team hopes to test its stimulation protocol in VCPs that have a greater number of implanted electrodes – hundreds to thousands as opposed to the 60 used in the current device. The researchers also want to work with computer vision specialists, engineers and visual neuroscientists to optimize algorithms that could be used to convert a camera image into dynamic stimulation sequences, which could convey entire visual scenes to the patients.
“This would mean continuously updating and identifying each of the salient objects and contours in the scene, and converting these into dynamic sequences that would be delivered to the electrode array in an interlaced fashion,” Bosking explains. “We hope that these techniques will prove useful in future VCPs no matter what type of electrodes or other stimulation technologies are used.”



