Radiation therapy plays an integral role in the management of breast cancer. Following breast-conserving surgery, in which the tumour is removed while leaving as much healthy breast tissue as possible, irradiation of the whole breast is a standard follow-up procedure. In some cases, irradiation of regional lymph nodes and/or a boost to the tumour cavity are also performed.
As survival rates improve for patients with early breast cancer, it’s important to consider potential long-term complications for those undergoing such radiation treatments. In particular, irradiation of the left breast is challenging due to the possibility of delivering dose to the heart and the subsequent risk of long-term cardiac complications.
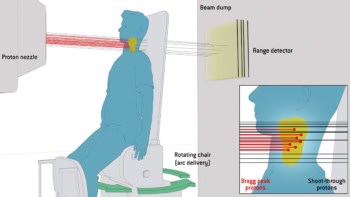
One way to reduce this risk is via the deep inspiration breath-hold (DIBH) technique, which physically separates cardiac structures from the target volume and helps reduce cardiac dose. Proton therapy can also be employed to help reduce cardiac dose, as protons target the tumour with high conformality while delivering almost zero dose to distal structures.
Researchers from the Rutgers Cancer Institute of New Jersey propose that combining the two techniques could reduce cardiac dose further. As previous studies of proton therapy with DIBH are scarce, they have compared photon DIBH with proton DIBH in 10 patients, reporting their findings in the International Journal of Particle Therapy.
Dose comparisons
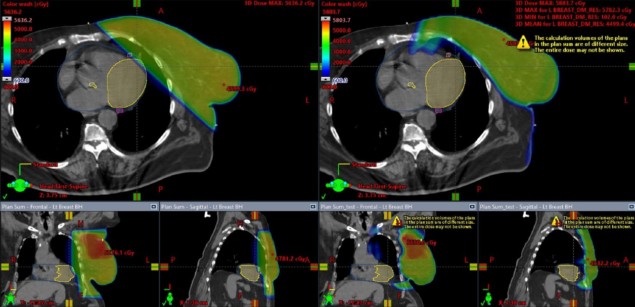
The study included 10 patients with left-sided breast cancer who received radiation as part of breast-conserving therapy. All underwent lumpectomy, nine also had sentinel lymph node biopsy and one underwent axillary lymph node dissection. All patients then received photon DIBH with two parallel, opposed beams used to irradiate the whole breast. Most patients also received a boost dose to the tumour cavity and, where required, nodal irradiation.
The researchers also created treatment plans for double-scatter proton therapy with DIBH, using clinical target volumes adjusted to match those of the delivered photon plans. Using each patient’s photon plan as a control for their proton plan, they investigated the doses to a number of cardiac subunits, including the entire heart, left ventricle (LV), left coronary artery (LCA), right coronary artery (RCA), left circumflex coronary artery (LCx) and left anterior descending coronary artery (LAD).
Both plan types provided adequate target coverage, but proton DIBH significantly reduced doses to cardiac structures compared with photon DIBH. This included reductions in: the mean dose to the heart (1.19 to 0.23 Gy); the mean dose to the LV (1.7 to 0.25 Gy); the mean, maximum and half-maximum doses to the LAD (5.54 to 1.15 Gy, 22.15 to 7.7 Gy, 4.42 to 1.61 Gy); and the maximum dose to the LCx (1.35 to 0.13 Gy).
The team point out that the lower mean doses to the entire heart, LV and LAD could lead to an estimated reduction in long-term cardiac mortality of at least 7%. The mean doses to the LCx, LCA and RCA were already low for photon DIBH, thus the clinical significance of further dose reduction to these structures with protons is unknown.
Added lung protection
Radiation pneumonitis (lung inflammation arising from irradiation) is another area of concern when planning breast radiotherapy. The researchers observed that proton DIBH significantly lowered the dose to the left lung compared with photon DIBH. The mean left lung dose was reduced from 8.04 to 2.28 Gy, while volumes receiving 20 Gy and 5 Gy were reduced by 13% and 17%, respectively. Clinically, this lower lung dose from proton therapy may have long-term benefits.
The study also revealed that proton therapy reduced the maximum dose to the right breast, although the result was not statistically significant. The researchers note that skin dose was slightly higher with proton than photon therapy. While the difference was not statistically significant, they suggest caution in this regard.

Breath-hold technique reduces patient motion during radiotherapy
“Proton DIBH significantly reduces dose to vital organs-at-risk in comparison to photon DIBH in patients requiring whole-breast radiation and/or nodal irradiation,” the researchers conclude. “This may be the new standard-of-care in the future because of its significant long-term clinical benefits.”
They point out, however, that understanding the clinical implications of this dosimetric advantage requires a randomized study with long-term follow-up. In addition, the expected toxicity profile from such proton treatment is difficult to anticipate because of the lack of adequate long-term clinical experience. “We hope that the ongoing RADCOMP study will be able to answer such questions in the coming few years,” they write.