Phase transitions within protein-rich aerosols and droplets may protect viruses at low humidity levels, which could explain why respiratory diseases such as COVID-19 can often spread efficiently in dry air. That is the conclusion of Ryan Davis of Trinity University in Texas and colleagues, who have observed a structural transition in aerosols that occurs as humidity falls.
Respiratory pathogens spread between hosts in either micrometre-scale aerosols – which remain suspended in air currents like cigarette smoke – or in larger droplets, which slowly fall to the ground under gravity. Both are emitted by infected hosts coughing, talking, singing or simply breathing. They are subsequently inhaled by new hosts.
The humidity (more accurately, the relative humidity) in the respiratory system is typically 100%, so as soon as a particle is emitted its surrounding humidity is usually lower. Exposure to drier air might be expected to destroy viruses adapted to the warm, moist atmosphere of the lungs, but this is not always the case.
Most viruses’ viabilities in exhaled particles – including those of influenza and the Sars-CoV-2 virus that causes COVID-19 – vary with humidity in a curious U-shape. At close to 100% humidity, the viruses can survive for relatively long times, whereas at intermediate humidity their lifetimes are shorter. This is because in drier air water evaporates faster from the outside of an aerosol particle, leaving it more concentrated in non-volatile components such as sodium chloride. When these components become too concentrated, they disinfect the particle. However, after dropping to a minimum at 50-80% humidity, the viabilities of most viruses begin to increase as humidity decreases further. The reasons for this are not entirely clear.
Protective shall?
Previously, researchers have proposed that it could be due to efflorescence, in which the inorganic content of the particle crystallizes, encapsulating the virus in a protective shell. As the water is driven off, this manifests as a sharp decrease in the particle mass.
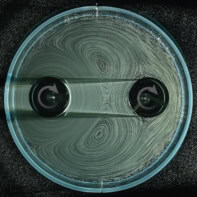
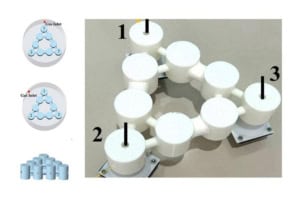
In the new research Davis and colleagues studied aerosols and droplets composed of model respiratory compounds (salt and protein) in growth media, which are organic–inorganic mixtures used in studies of pathogen survival. They showed that efflorescence was suppressed, sometimes to humidity levels as low as 35%. However, when they tried to merge levitated particles together, they found many of them behaved as solids or semi-solids at much higher humidity, with the firmness of the particles gradually – and unexpectedly – increasing as the humidity fell.
The researchers believe, therefore, that they were observing glass transitions due to cross-linking of the organic molecules in the growth media. “Glass transitions happen over a broad range,” explains Davis. “And when you have a glass transition, molecular motion kind of stops. That’s one reason why we think a glass transition could cause long virus survival times – because whatever inactivation process happens is going to be slowed down.”
Complex, elongated shapes
In a growth medium that contained calcium ions, however, the particles coalesced fully at humidity levels above 53%, below which they formed complex, elongated shapes. When the researchers looked at these under a microscope, they found that the particles had separated into liquid and solid fractions. They attribute this to a phase transition, in which the calcium crosslinks the proteins in the solution to form a gel.
“You can have what’s called a critical gel concentration fairly abruptly,” says Davis. “The proteins and the viruses likely do migrate together and partition into the organic phase where that organic can form a rigid protective layer.” An important subtlety is that small aerosols are likely to reach a protective state in seconds after emission as evaporation will occur quickly, whereas larger droplets may have been sterilized by the time it forms.
Droplets created by speech could contribute to COVID-19 spread, new study suggests
The researchers conclude that the organic content of the encapsulating particle is probably crucial to viruses’ viability at any given humidity. This organic content will depend upon where in the respiratory tract the particle was produced, which in turn will depend on the disease and how far it has progressed in a specific patient. “The next step would be to systematically vary different aspects of the droplet composition and the virus involved to try to understand better what the mechanism of viral deactivation is,” says Davis.
Biological aerosol expert Peter Raynor of the University of Minnesota in the US says “I think it’s an important [study], but there have been important [studies] before this and there are going to need to be important [studies] after this to give us a complete picture of how droplet composition is linked to survivability.” He adds, “Potentially an important outcome of this line of research is making sure we properly humidify buildings in the winter when otherwise there would be dry air, not only for human comfort but also to keep viruses in their most fragile state.”
The research is described in Proceedings of the National Academy of Sciences.