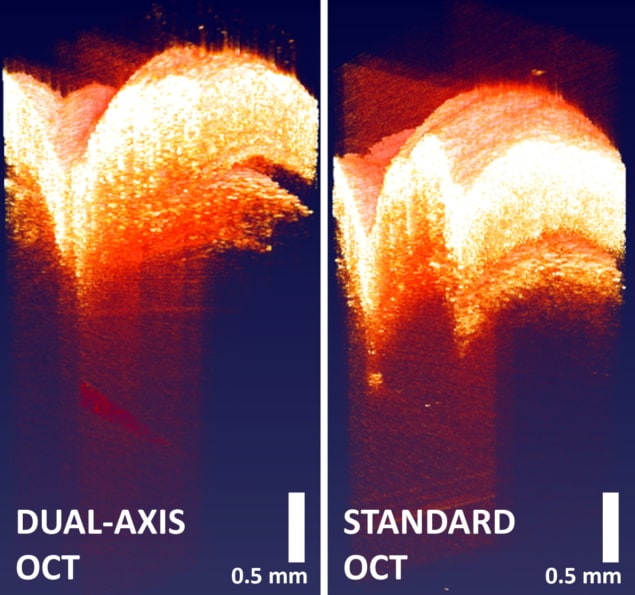
Biomedical engineers at Duke University have developed a new dual-axis optical coherence tomography (DA-OCT) system that increases the imaging depth by almost 50% compared with conventional OCT. This ability to reach deeper layers of tissue could enable the use of OCT to assess burn damage to skin, examine healing processes or help diagnose skin cancer.
OCT is widely used in ophthalmology, but its use in dermatology has been limited by the technique’s inability to obtain clear images beyond a depth of about 1 mm. The new DA-OCT system, described in Biomedical Optics Express, combines the inherently reduced scattering offered by a 1.3 µm light source with the depth enhancement afforded by a dual-axis geometry, The outcome: improved signal contrast with significantly increased penetration depth over previous DA-OCT approaches.
The new technique works by directing light onto the object being imaged at a slight angle. The detector is set up at an equal and opposite angle, creating a dual-axis configuration. This allows the detector to benefit from the slight scattering angle introduced by the object’s physical nature. “By tilting the light source and detector, the chances of collecting more of the light that is scattering off at odd angles from a tissue’s depths can be increased,” explains first author Evan Jelly.
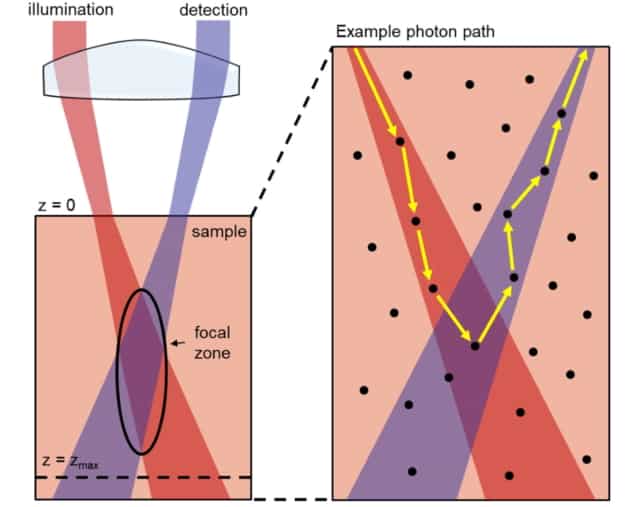
Jelly discovered that the depth of the focal point of light within the tissue makes a large difference to how well this dual-axis approach works in OCT. Because the axial field-of-view inherently decreases as the angle increases, he devised a method of scanning the focus of the narrower window through various tissue depths, and then combining the data into a single image. The technique uses a tunable lens to coordinate focal plane selection with image acquisition, enabling DA-OCT with an enhanced depth-of-focus (DOF).
The DA-OCT design utilizes a custom spectrometer design based on a low-cost architecture and incorporating a micro-electromechanical systems (MEMS) mirror for fast beam scanning. Graphics processing unit-assisted processing produces a frame rate of approximately 20 frames per second, with volumetric imaging performed in seconds. The team used a previously developed dual-window speckle reduction method to achieve real-time speckle reduction.
System characterization
To compare DA-OCT against conventional OCT, Jelly and colleagues used both methods to image a complex tissue phantom – mimicking several layers of skin, fat and fascia – containing an inserted 28-gauge needle. They also imaged laboratory mice with a needle inserted through the skin.
The researchers employed four imaging modes: conventional on-axis OCT; DA-OCT; on-axis OCT with enhanced DOF; and DA-OCT with enhanced DOF. In phantoms, they performed enhanced DOF imaging by scanning the optical focus from 500 to 1400 µm at 100 µm increments and stitching the images together during post-processing. For imaging in tissue, the researchers acquired repeated image frames with the focus of the tunable lens placed at 500 μm (3 frames), 750 μm (3 frames) and 1000 μm (4 frames). These images were compiled to create 10-frame averaged scans with an enhanced DOF.
Principal investigator Adam Wax reports that the dual-axis architecture provided improved penetration capability in both phantoms and mouse skin compared with conventional on-axis OCT. The dual-axis OCT was able to image the tip of a needle 2 mm beneath the murine skin surface, compared with 1.2 mm considered to be the traditional landmark depth of conventional OCT.

The resolution of the DA-OCT system was similar to that of a conventional OCT system when no scattering tissue was present, though resolution was degraded after multiple scattering events. However, the researchers showed that DA-OCT allows contrast from deep objects to be preserved when DOF enhancement is applied. They also note that while the focal zone of the DA-OCT system near 1–2 mm into the skin provides better image contrast than a co-axial OCT system, this enhancement depends on maintained overlap between illumination and detection beam foci.
Additionally, the researchers determined that the advantages of DA-OCT are only realised when anisotropy is high, as in many biological tissues. They note that while imaging at 1.3 µm inherently increases penetration, the reduction of tissue anisotropy at the 1.3 μm wavelength limits the additional benefit of DA-OCT.
Contrast-enhanced OCT visualizes vascular leakage in the retina
“This research helps us better understand the underlying principles driving our technique and provides a roadmap for situations where dual-axis OCT may be applied for superior depth penetration,” Jelly explains.
The team has subsequently developed a portable device that can be administered at the point-of-care. “This involved engineering a robust handheld device that maintains extremely highly optical tolerances needed to keep the overlap between the two beams, which produce the DA-effect,” says Jelly. “Preliminary designs for the technology are currently in the early stages of development for dermatological and dental applications.”