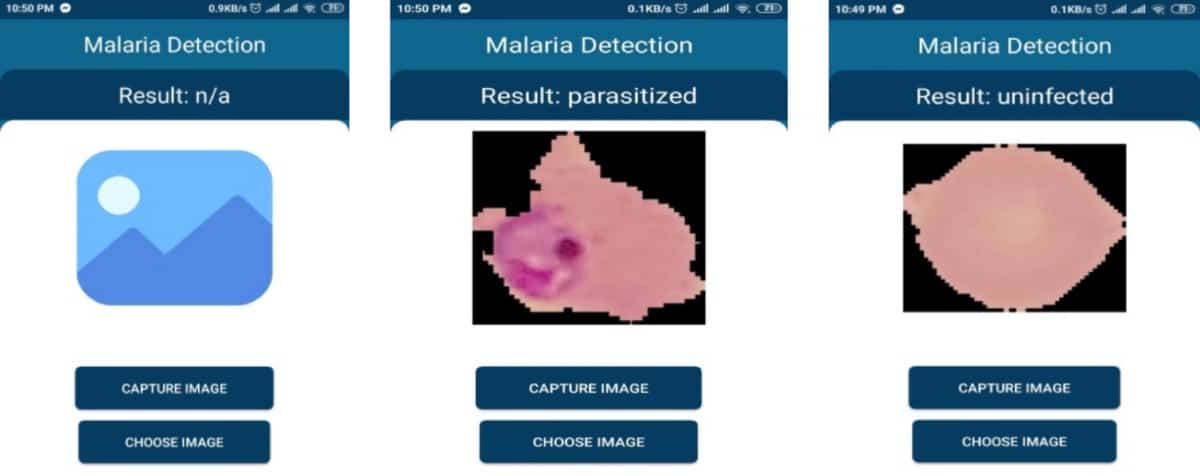
A team of six engineers from the North South University of Bangladesh has developed a program that can automatically diagnose malaria using a smartphone presented with a segmented blood smear image. This approach has potential to overcome the need for expensive equipment and highly trained personnel for malaria diagnosis in resource-limited settings. If patient samples, so-called blood smears, are imaged using a mobile phone and microscope, then the app can analyse the images for the presence of malaria parasites.
Writing in the journal Diagnostics, the developers explain that “the model can work independently in the mobile app without needing Internet connection and can help an individual without any technical expertise to detect malaria parasites from the blood smear”.
The research team developed 10 computational models and evaluated their computational requirements, as well as their accuracy, precision, sensitivity and specificity. Some of the models were trained using autoencoder, a type of artificial neural network used to learn in an unsupervised manner how to detect patterns while disregarding noise. These autoencoder-trained models were the smallest in size at just 73 KB (less than Whatsapp). Such computational efficiency enables automatic diagnosis to be performed on low-cost smartphones.

From computational heavy to lightweight
In 2019, engineers from the US had already developed a neural network that could achieve automatic malaria diagnosis. However, their model was too computationally intensive to work on smartphones or in a web browser. The new model by Faizullah Fuhad and his colleagues requires over 4 million times less processing capacity than the previous model while maintaining very high classification accuracy. The team from Bangladesh demonstrated functionality both offline on mobile phones, as well as online in a web application.
The researchers used a public dataset containing 27,558 images of red blood cells from 150 infected and 50 healthy patients to train the model. The images were taken by placing a smartphone on a conventional light microscope (available from approximately £100). Afterwards, the developers tested the model on a different public dataset, confirming the model’s robust performance.
The pros and cons of diagnosis methods
Currently, malaria can be diagnosed from clinical symptoms such as fever, or by polymerase chain reaction (PCR), rapid diagnostic test (RDT) or microscopy. As clinical diagnosis and PCR require laboratory settings, the other two methods, RDT and microscopy, are most commonly used for malaria diagnosis today.
RDT is a powerful tool, using a test strip similar to a pregnancy test. However, this method has some shortcomings compared with microscopy. It is less sensitive, more expensive and affected by heat and humidity. Also, RDT can neither quantify parasite density nor identify the species of parasite causing the infection. Microscopy is therefore the best available technique, but unfortunately requires highly trained personnel. The new smartphone app developed by Fuhad and colleagues should overcome this limitation.



