Researchers in Australia have made a new type of imaging needle that can be used during brain biopsies to detect cerebral blood vessels. The device, which is the first of its kind, works thanks to an optical coherence tomography camera attached to the needle and could reduce the risk of fatal haemorrhaging during neurosurgery. It has already been successfully tested out in vivo on 11 human patients.
“We start off with an optical fibre around 125 microns thick and build a tiny lens on the end of it,” explains Robert McLaughlin of the University of Adelaide, who led this research study. “We then angle-polish the end of the lens so that light will come out at its side. We then glue this fibre-optic probe into a commercial brain biopsy needle.
“Standard biopsy needles have a hole at the side, near the tip, and this is where they suck the tissue that is to be removed from the brain for subsequent testing and diagnosis. Our probe ‘looks out’ through this hole so that it can warn the neurosurgeon if they are about to cut a blood vessel.”
Roughly 80,000 people are diagnosed with primary brain tumours each year in the US alone and 14,000 of these patients undergo brain biopsies. Although the procedure is minimally invasive, it still carries a risk because there is a chance that the needle will damage an important vessel. Indeed, about 1% of patients die and 2-3% are left disabled following this damage.
Optical coherence tomography to detect blood vessels
McLaughlin and colleagues’ needle makes use of optical coherence tomography (OCT) to detect blood vessels by differentiating this tissue from blood that is flowing. OCT is similar to ultrasound but uses light waves instead of sound waves.

The technique is routinely employed in ophthalmology and cardiology and does not require any fluorescent or other labels. It instead measures the light scattered from tissue when it is illuminated using near-infrared light. Researchers reconstruct the backscattered optical signal into a structural image of the tissue, and spatial resolutions of 5 to 20 microns are possible.
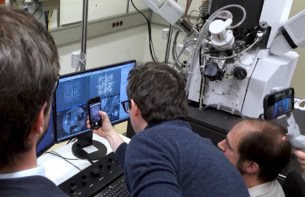
“Flowing blood has a particular characteristic appearance in these images,” says McLaughlin. “We developed an intelligent image processing algorithm to distinguish between this blood and stationary brain tissue. During neurosurgery the surgeon can see the scan in real time and our software marks it in red when the needle is next to a blood vessel.”
Two types of studies
“One of the major challenges in this work was to determine how accurately the needle could detect blood vessels that can’t be seen with other, standard imaging methods such as magnetic resonance imaging (MRI) because they are too small,” he explains. “We thus performed two types of studies.
“We tested the needle out on 11 patients, all of whom were undergoing craniotomies as part of other types of surgery,” he explains. “This is where the surgeon removes a part of the skull to reveal the brain, so we could see the blood vessels on its surface. For each patient, we chose several blood vessels and moved the needle over the vessel to see if the needle could detect it. We then moved the device over areas without blood vessels to make sure nothing was being detected. This is how we were able to calculate that the needle has a sensitivity of 91.2% and a specificity of 97.7% in blood vessels measuring more than 500 microns across.”
For three of the patients (with grade IV astrocytoma), McLaughlin’s team also deeply inserted the needle into brain tissue – as is done in a normal biopsy. “Before this particular surgery, we identified a blood vessel that was visible on an MRI scan of the patient’s head. We then drilled a small hole in their skull and inserted the needle so that it was adjacent to the blood vessel. In all three cases, the needle was able to detect that it was indeed next to the blood vessel.” This is how the researchers were able to calculate that the needle can detect blood vessels at depths of 21.9 mm, 25.3 mm and 27.2 mm.
“The patients were at Sir Charles Gairdner Hospital in Western Australia and of course gave their consent to be part of this study and weren’t undergoing biopsies,” McLaughlin tells Physics World. “They were actually having other types of brain surgery and in all cases were going to have a diseased part of their brain removed. It was very important for us to come up with a way to test this new device without putting the patient at any risk at all. So, for each patient, we only did experiments on parts of the brain that were going to be removed.”
More advanced needle could detect cancerous tissue too
“Ours is the first reported use of such a probe in the human brain during live surgery and is the first step in the long process required to bring new tools like this into clinical practice,” he adds. “There are many types of operations where a needle is inserted into tissue and there is risk of a bleed, but brain biopsies are the most important because the impact of bleeds in the brain can be so catastrophic.”
The researchers, reporting their work in Science Advances 10.1126/sciadv.aav4992, say they are now working on a version of their needle that can detect cancerous tissue as well as blood vessels. “In current practice, a neurosurgeon may take eight to ten tissue samples during a brain biopsy using a standard needle. If we can develop a needle that can detect when it is in cancerous tissue, they may then only need to take one sample, which would be much safer.
“Developing the next generation of such needles will take several more years of research and development because we need to be very careful when developing tools that will be used on patients.”