A microelectrode array implanted in the visual cortex of a blind woman enabled her to attain a simple form of vision and identify lines, shapes and letters. In a six month clinical investigation at the University Miguel Hernández in Spain, the Utah Electrode Array (UEA) demonstrated high potential for restoring a useful sense of vision in sightless individuals and increasing their independence.
Berna Gómez, a 60-year old former science teacher who developed toxic optic neuropathy causing total blindness 16 years previously, volunteered to work with scientists from the John A. Moran Eye Center at the University of Utah and Eduardo Fernández from University Miguel Hernández. Gómez is the first person to have the UEA implanted in the visual region of the brain for an extended period of time and to undergo repeated stimulations.
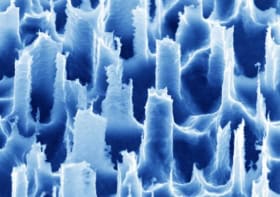
Co-principal investigator Richard Normann, a University of Utah bioengineer, developed the first UEA 30 years ago. The device comprises a 100 microelectrode array implanted into the brain to record and stimulate the electrical activity of neurons, with the goal of restoring useful vision to blind people.
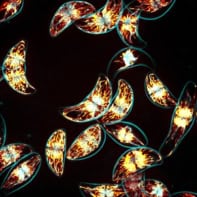
For this study, reported in the Journal of Clinical Investigation, the team used the experimental Moran/Cortivis Visual Prosthesis, which includes a pair of glasses equipped with a miniature video camera that transmits images in real time. The visual data collected by the camera are encoded by specialized software and sent it to the UEA. The array then stimulates neurons to produce phosphenes (flashes of light seen without visual input), perceived by Gómez as white points of light, to create an image.
To optimize the implantation location of the electrode array, the researchers used MR imaging prior to surgery to create a three-dimensional reconstruction of the surface anatomy and neurovascular structures of the subject’s primary visual cortex. They selected a region of the right occipital cortex that could be accessed easily while avoiding major blood vessels.
A neurosurgeon performed a craniotomy centred over the desired location, and implanted the 4 mm square UEA with 96 microelectrodes projecting out from its silicon base. The electrode’s external connector was attached to the skull using six titanium microscrews. Gómez underwent electrical stimulation and multiunit neural recording sessions once or twice daily, five days a week, for up to four hours per session. Over the six month study period, she received approximately 540 hr of stimulation.
Identifying the light
Because blind people often experience random flashes of light, called spontaneous phosphenes, Gómez was trained to differentiate these from the electrically-induced phenomena. In the first days after implantation, she reported one episode ever 5–10 s, but after 12 weeks, these occurred only occasionally. During the nearly two-month training period, she learnt to recognize that the electrically-induced phosphenes were always localized to the same general region of her visual space, and that they appeared in conjunction with a low-frequency auditory tone used to indicate the start of electrical stimulation.
The researchers determined that increasing the number of stimulating electrodes, from two to 16, significantly increased the perceived brightness, clarity and size of the phosphenes. They observed that it was easier for Gómez to “see” spots of light when more than two electrodes were stimulated. Spacing out the stimulating electrodes also improved recognition of shapes and letters, with electrodes spaced 400 µm apart able to generate separate distinct images.
Gómez was then able to identify multiple letters and to differentiate whether they were upper or lower case. She also was also able to discriminate between different patterns and/or groups of electrodes when playing a specially designed video game.
The team found that the colour and brightness of perceived images could be controlled by adjusting the electrical current used to stimulate individual microelectrodes. Currents above 50% of the threshold stimulus level (66.8±36.5 µA for a single electrode) produced brighter and whiter light; lower currents created dim images of a sepia colour. The highest brightness ratings were reached with currents of about 90 μA.
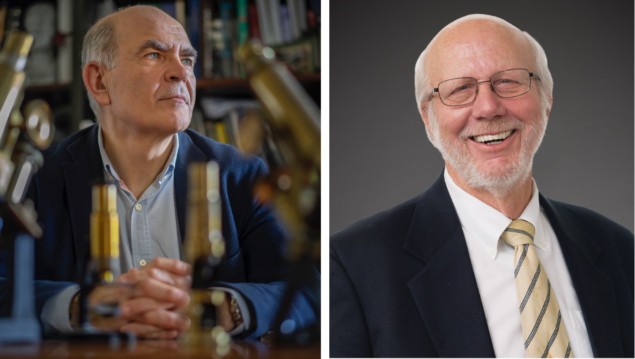
“These results are very exciting because they demonstrate both safety and efficacy,” comments Fernández, who has collaborated with Normann for more than 30 years. “We have taken a significant step forward, showing the potential of these types of devices to restore functional vision for people who have lost their vision.”
“One goal of this research is to give a blind person more mobility,” adds Normann. “It could allow them to identify a person, doorways or cars easily. It could increase independence and safety. That’s what we’re working toward.”
The team hopes that the next set of experiments will use a more sophisticated image encoder system, capable of stimulating more electrodes simultaneously to reproduce more complex visual images. They explain that a single UEA array is unlikely to be sufficient for useful vision. “In the future, we expect that several arrays of intracortical microelectrodes would be tiled across the visual cortex, permitting phosphene induction across a larger area of the visual field and forming the basis for functional sight restoration.”