Dense breast tissue can mask cancers on mammograms, making screening more difficult, and is also an independent risk factor for breast cancer. Now, researchers from Massachusetts Institute of Technology (MIT) and Massachusetts General Hospital (MGH) have developed a deep-learning algorithm that assesses breast density in mammograms as reliably as an experienced mammographer (Radiology 10.1148/radiol.2018180694).
In the USA, many states have laws mandating that women are notified if their mammograms indicate dense breast tissue. But breast density assessments rely on human assessment and results can vary among radiologists. “We’re dependent on human qualitative assessment of breast density, and that approach has significant flaws,” explains lead author Constance Lehman from MGH. “We need a more accurate tool.”
“Our motivation was to create an accurate and consistent tool that can be shared and used across health care systems,” adds Adam Yala, a PhD student in MIT’s Computer Science and Artificial Intelligence Laboratory.
Every mammogram has a BI-RADS breast density rating in one of four categories: fatty; scattered fibroglandular; heterogeneously dense; or dense. The researchers developed a model, is built on a deep convolutional neural network, that can distinguish the different categories of breast tissue.
The researchers trained and tested the algorithm on a dataset of more than 58,000 digital screening mammograms. They used around 41,000 mammograms for training and about 8600 for testing. During training, the algorithm is given random mammograms to analyse and learns to map the mammogram with the original radiologist’s interpretation. Given a new mammogram, it can then predict the most likely density category.
Clinical application
In January of this year, the deep-learning algorithm was implemented in routine clinical practice at MGH. In a traditional workflow, mammograms are sent to a workstation for a radiologist to assess. For this study, the algorithm was applied first to assign each mammogram a density rating. Then when radiologists view a scan at their workstations, they see the model’s assigned rating, which they can then accept or reject.
The researchers note that this marks the first time that this type of deep-learning model has successfully been used in routine clinical practice. “It takes less than a second per image … [and it can be] easily and cheaply scaled throughout hospitals,” says Yala.
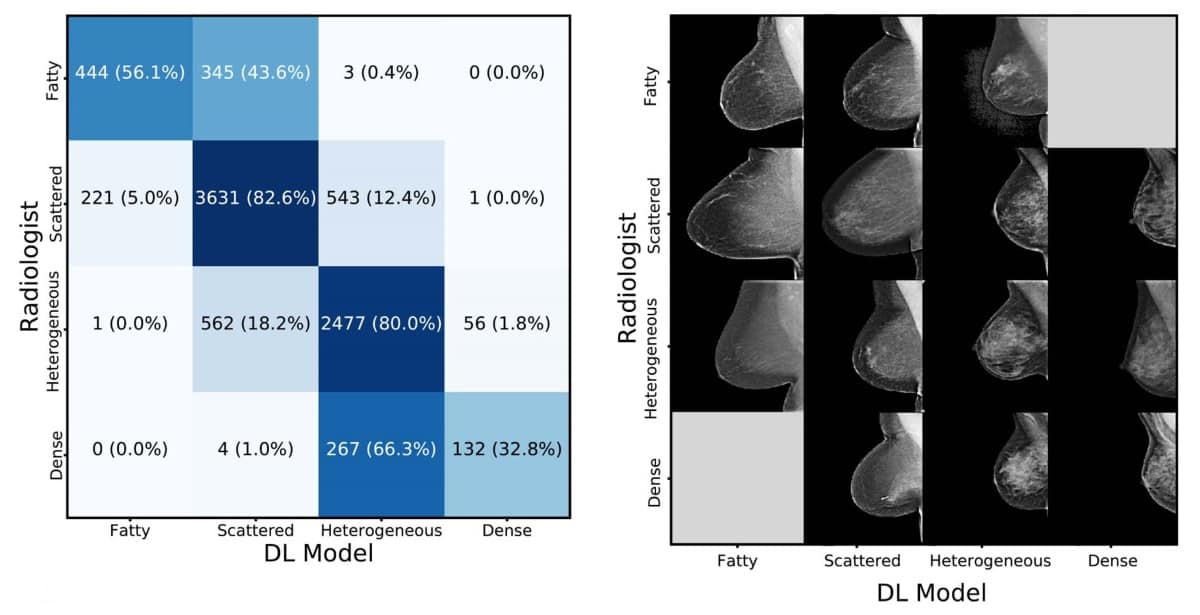
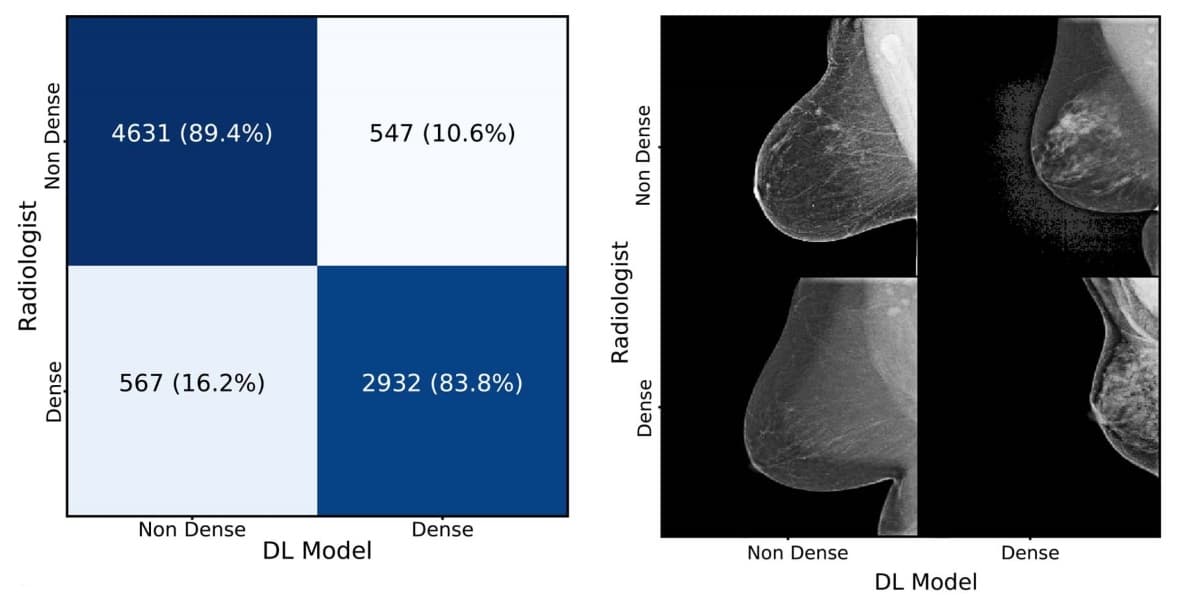
The study reports on 10,763 consecutive mammograms assessed by the algorithm and reviewed by eight radiologists. In a binary test determining whether breasts were heterogeneous and dense, or fatty and scattered, the algorithm achieved 94% agreement with the radiologists. Across all four BI-RADS categories, it matched radiologists’ assessments at 90%.
“We were thrilled with the results,” says Lehman. “Now at Mass General, the deep-learning algorithm processes all our screening mammograms and provides density, which is either accepted or rejected by the radiologists.”
The algorithm has the potential to standardize and automate routine breast density assessment. On a broader scale, the researchers see artificial intelligence (AI) as central to the development of personalized breast cancer risk assessment. AI is uniquely suited to breast imaging because it can draw upon a large, mature database with advanced, structured reporting that links images with outcomes.
“With AI, we now have the ability to leverage vast amounts of information into more personalized, more targeted care for our patients,” says Lehman. “In the case of breast cancer, we can better predict how likely a woman will have cancer in her future and improve the chances that it will be treated successfully.”



