The importance of innovative thinking in healthcare services the world over is paramount – new treatments, technology and processes could make a real difference to patients. Yet, in many national structures, it is often complicated and difficult to actually enable new techniques and technologies to reach the end-users. The UK’s National Health Service (NHS), for example, is struggling to deliver on its innovation agenda.
The NHS, and the UK Government, has initiated a number of financial initiatives, prompted by an Accelerated Access Review published in October 2016. But these have not yet had the desired impact. When it comes to finding local routes to market, regardless of the geography, it’s not all about the money.
In services constrained by capacity issues, developing the capability, culture and creative partnerships required to innovate is crucial to success. The NHS, for example, is full of exceptionally talented and hard-working staff who, in the course of their daily delivery of care to their patients, are working with sub-optimal technologies and processes that could be improved to deliver better services to patients. Capturing these unmet needs and translating them into new life-enhancing technology solutions is the challenge.

Health Enterprise East (HEE) is an example of the sort of body that can help identify these needs; it was set up 13 years ago to help dedicated healthcare staff translate their ideas for new medical technologies into reality. HEE provides professional advice to a network of 30 NHS organizations on patents and intellectual property protection. It also provides access to proof-of-concept funding and support in finding the most appropriate route to market.
Spin-out success
In many countries, there has historically been a lack of funding for early-stage proof-of-principle work. But by working with bodies such as HEE, there is the opportunity to not only help patients, but also support the economic growth agenda in the form of jobs, revenues and the scope to leverage inward investment. Backed by £11m of development funding through HEE’s Medtech Accelerator and Medovate initiatives (set up by HEE with public and private sector partners), HEE ensures that innovations from NHS staff that show the greatest promise can be supported through early-stage feasibility studies to regulatory approval and first-in-man clinical studies.
There are countless innovators working in health services. This is evidenced by the roughly 200 innovation disclosures that HEE receives each year from NHS staff, exploring the commercial potential of these either through a licensing route (to an existing manufacturer or distributor) or the creation of a spin-out company.

And these spin-outs can thrive – one of HEE’s most successful spin-out companies is EarFold, a pioneering implant technology that provides an alternative to conventional otoplasty surgery in the correction of prominent ears. A minimally invasive technique, the procedure takes 20 minutes under local anaesthetic as an outpatient, compared with the traditional two hours in surgery, and overall patient outcomes are improved. It’s an example of a simple innovation that ticks all the boxes in terms of improving patient care, and is cheaper and safer.
The technology was spun out of West Hertfordshire NHS Foundation Trust in 2010, raising around £1.1m in external investment. HEE invested over £100k to prove the concept, secure patents internationally, undertake detailed market research and define a product development plan. EarFold received a CE mark in April 2015, prior to its parent company Northwood Medical Innovation being acquired by global pharma Allergan in October 2015.
Another example of pioneering innovation is Ablatus Therapeutics, which is commercializing a novel tissue ablation technology to treat the most challenging, and often inoperable, solid cancer tumours. With support from HEE, the company was spun-out of Norfolk & Norwich University Hospitals NHS Foundation Trust, where the technology originated, and has received over £2m investment to date.
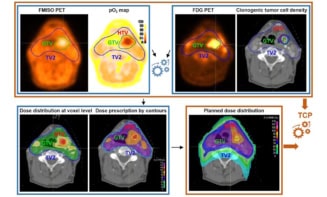
Tissue ablation is a surgical procedure used to destroy tissue, such as a tumour, in situ. A needle-like probe is placed inside the tumour; radiofrequency waves passing through the probe increase the temperature within the tissue and result in tumour destruction. Current application of the procedure, however, is limited in terms of the size and location of tumours that can be treated. Ablatus is using a novel technology called bimodal electric tissue ablation (BETA) to address some of the existing problems and increase the size of the treatment zone compared with other technologies.
Nurturing start-ups
Funding initiatives like Medtech Accelerator and Medovate encourage more public-private investment into the healthcare innovation landscape, supporting development of new technologies at greater pace and scale. The question remains: how do you achieve uptake of these ideas into a fragmented service, constrained by resources, where innovation is often stifled at source?
The NHS spends over £1bn on research and development, through the National Institute for Health Research (NIHR), but only a fraction of that on the adoption and diffusion of good ideas. To support the development of the skills and capability required for change, clinicians can now get paid time away from clinical duties, in addition to being given access to mentors and other networking opportunities, through the National Clinical Entrepreneurs programme.
Expanding on this programme and others like it, and ensuring greater co-ordination and accountability across the various initiatives, will support medical staff to work with technology and business experts to deliver on innovation agendas.
Another important player in the landscape, providing further evidence of how start-ups can be nurtured, is NHS England’s SBRI Healthcare programme. Led by the 15 Academic Health Science Networks (AHSNs) across England, SBRI Healthcare works with local clinical networks to identify needs and then funds technology companies to develop solutions.
In the last five years, the programme has dispersed funding of £73m to innovative technology companies to develop solutions for unmet needs. Solutions now on the market include MyCOPD, a digital tool to help patients with chronic obstructive pulmonary disease better self-manage their condition through “My mHealth” app, and the Patient Status Engine, a continuous wireless patient monitoring platform from digital healthcare business Isansys.
A recent independent review of the benefits from the programme indicated that projects had secured savings to date to the healthcare system of between £24.6 and £30.1m. This is despite the early assessment of returns – new medical technologies typically take between three and eight years just to reach market. The small and medium sized companies (SMEs) funded through the programme work closely with the AHSNs to really understand both the clinical needs and business case required to secure successful adoption of solutions when they come to market.
These creative partnerships with SMEs, often identified as the engines of UK economy growth, are just some examples of the new ways that health services can work with industry to meet its innovation aims. Such tactics must be encouraged if our health services are to achieve the modernity and cutting-edge technology they merit.