Researchers at the University of Victoria in Canada are developing a low-cost radiotherapy system for use in low- and middle-income countries and geographically remote rural regions. Initial performance characterization of the proof-of-concept device produced encouraging results, and the design team is now refining the system with the goal of clinical commercialization.
This could be good news for people living in low-resource settings, where access to cancer treatment is an urgent global health concern. The WHO’s International Agency for Research on Cancer estimates that there are at least 20 million new cases of cancer diagnosed annually and 9.7 million annual cancer-related deaths, based on 2022 data. By 2030, approximately 75% of cancer deaths are expected to occur in low- and middle-income countries, due to rising populations, healthcare and financial disparities, and a general lack of personnel and equipment resources compared with high-income countries.
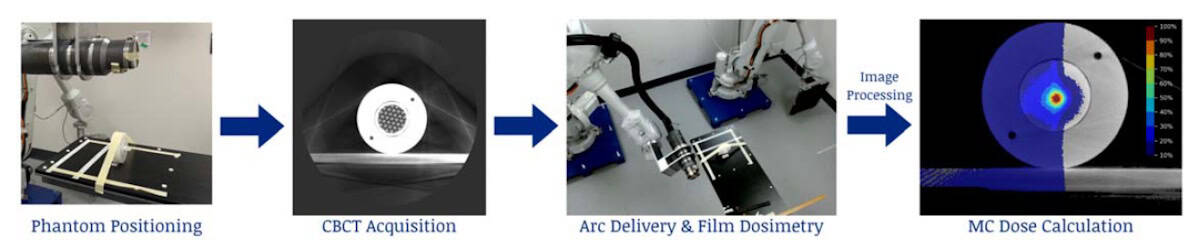
The team’s orthovoltage radiotherapy system, known as KOALA (kilovoltage optimized alternative for adaptive therapy), is designed to create, optimize and deliver radiation treatments in a single session. The device, described in Biomedical Physics & Engineering Express, consists of a dual-robot system with a 225 kVp X-ray tube mounted onto one robotic arm and a flat-panel detector mounted on the other.
The same X-ray tube can be used to acquire cone-beam CT (CBCT) images, as well as to deliver treatment, with a peak tube voltage of 225 kVp and a maximum tube current of 2.65 mA for a 1.2 mm focal spot. Due to its maximum reach of 2.05 m and collision restrictions, the KOALA system has a limited range of motion, achieving 190° arcs for both CBCT acquisition and treatments.
Device testing
To characterize the KOALA system, lead author Olivia Masella and colleagues measured X-ray spectra for tube voltages of 120, 180 and 225 kVp. At 120 and 180 kVp, they observed good agreement with spectra from SpekPy (a Python software toolkit for modelling X-ray tube spectra). For the 225 kVp spectrum, they found a notable overestimation in the higher energies.
The researchers performed dosimetric tests by measuring percent depth dose (PDD) curves for a 120 kVp imaging beam and a 225 kVp therapy beam, using solid water phantom blocks with a Farmer ionization chamber at various depths. They used an open beam with 40° divergence and a source-to-surface distance of 30 cm. They also measured 2D dose profiles with radiochromic film at various depths in the phantom for a collimated 225 kVp therapy beam and a dose of approximately 175 mGy at the surface.
The PDD curves showed excellent agreement between experiment and simulations at both 120 and 225 kVp, with dose errors of less than 2%. The 2D profile results were less than optimal. The team aims to correct this by using a more optimal source-to-collimator distance (100 mm) and a custom-built motorized collimator.
Geometrical evaluation conducted using a coplanar star-shot test showed that the system demonstrated excellent geometrical accuracy, generating a wobble circle with a diameter of just 0.3 mm.
Low costs and clinical practicality
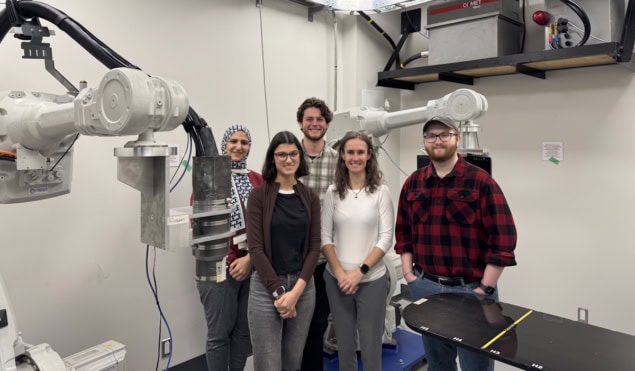
Principal investigator Magdalena Bazalova-Carter describes the rationale behind the KOALA’s development. “I began the computer simulations of this project about 15 years ago, but the idea originated from Michael Weil, a radiation oncologist in Northern California,” she tells Physics World. “He and our industrial partner, Tai-Nang Huang, the president of Linden Technologies, are overseeing the progress of the project. Our university team is diversified, working in medical physics, computer science, and electrical and mechanical engineering. Orimtech, a medical device manufacturer and collaborator, developed the CBCT acquisition and reconstruction software and built the imaging prototype.”
Masella says that the team is keeping costs low is various ways. “Megavoltage X-rays are most commonly used in conventional radiotherapy, but KOALA’s design utilizes low-energy kilovoltage X-rays for treatment. By using a 225 kVp X-ray tube, the X-ray generation alone is significantly cheaper compared to a conventional linac, at a cost of USD $150,000 compared to $3 million,” she explains. “By operating in the kilovoltage instead of megavoltage range, only about 4 mm of lead shielding is required, instead of 6 to 7 feet of high-density concrete, bringing the shielding cost down from $2 million to $50,000. We also have incorporated components that are much lower cost than [those in] a conventional radiotherapy system.”
“Our novel iris collimator leaves are only 1-mm thick due to the lower treatment X-ray beam energy, and its 12 leaves are driven by a single motor,” adds Bazalova-Carter. “Although multileaf collimators with 120 leaves utilized with megavoltage X-ray radiotherapy are able to create complex fields, they are about 8-cm thick and are controlled by 120 separate motors. Given the high cost and mechanical vulnerability of multileaf collimators, our single motor design offers a more robust and reliable alternative.”
The team is currently developing a new motorized collimator, an improved treatment couch and a treatment planning system. They plan to improve CBCT imaging quality with hardware modifications, develop a CBCT-to-synthetic CT machine learning algorithm, refine the auto-contouring tool and integrate all of the software to smooth the workflow.
Humanitarian engineering can improve cancer treatment in low- and middle-income countries
The researchers are planning to work with veterinarians to test the KOALA system with dogs diagnosed with cancer. They will also develop quality assurance protocols specific to the KOALA device using a dog-head phantom.
“We hope to demonstrate the capabilities of our system by treating beloved pets for whom available cancer treatment might be cost-prohibitive. And while our system could become clinically adopted in veterinary medicine, our hope is that it will be used to treat people in regions where conventional radiotherapy treatment is insufficient to meet demand,” they say.




