
A study published in the Annals of Neurology has shown that different types of aura – a common visual disturbance triggered during migraine – produce specific blood oxygen level-dependent (BOLD) functional MRI (fMRI) responses. Researchers at the University of Copenhagen induced positive (such as flashing lights) and negative (dark spots, for example,) aura symptoms in five patients with susceptibility to migraine with aura, and scanned the patients immediately afterwards. Their findings will help future work to characterize the clinical heterogeneity of migraine episodes and hence inform prognoses and therapeutic interventions (Annals of Neurology doi: https://doi.org/10.1002/ana.25096).
Approximately 10–30 % of migraine sufferers experience aura symptoms, typically in the premonitory phase of migraine (Migraine Trust). Negative visual symptoms include scotoma – where a portion of the visual field is degenerated/occluded – or dark spots, and positive visual symptoms include flashing lights/dots and zig-zag lines. Aura is thought to be caused by cortical spreading depression (CSD) – a wave of cortical depolarization, followed by suppression of neuronal activity, when headache typically ensues. Aura is a transient symptom that is difficult to characterize, and hence difficult to investigate. Here, researchers imaged participants across two non-consecutive study sessions using fMRI.
Inducing migraine with aura
On day 1, the researchers scanned five subjects at baseline and then during aura. One patient inhaled atmospheric air, and three were submitted to normobaric hypoxia – reduced O2concentration at normal atmospheric pressure – in order to induce aura. The remaining subject exercised on a bike while exposed to flickering photo-stimulation. fMRI was performed during stimulation with a moving checkerboard to strongly activate the visual cortex.
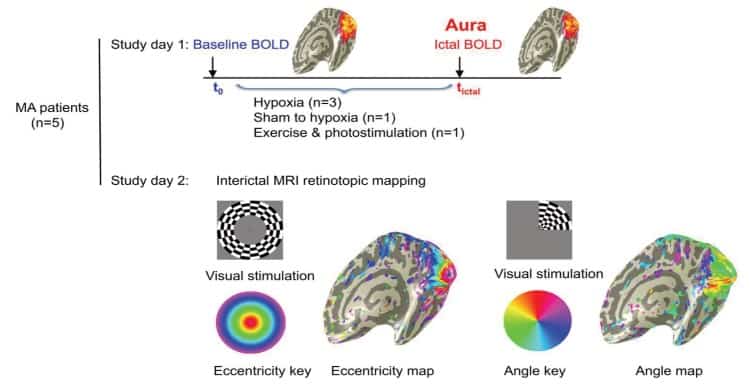
On day 2 (at least five days after an attack), the investigators performed retinotopy (visual cortex mapping while the subjects observed rotating wedges and expanding/contracting ring stimuli) to identify specific parts of the visual cortex.
Specific responses to specific aura
Two patients experienced scotoma/flickering, which corresponded to a reduced BOLD response (compared with baseline). One patient experienced black and white spots and flickering, and had a reduced BOLD response. The remaining two patients experienced white spots/flickering and had an increased BOLD response. Solely positive symptoms such as flickering/bright spots/lines increased the BOLD response. Several of these specific BOLD responses were present on both hemispheres, similar to the visual disturbances experienced by the patients.
In some cases, patients experienced a combination of positive and negative symptoms. In these patients only a reduced BOLD response was observed. The authors suggest this may be due to different effects of CSD on the cerebral activity and haemodynamics: positive symptoms may reflect the start of the wave of depolarization – the neurons are hyperexcitable and quickly regain resting potential – and negative symptoms may reflect the depressed areas after the wave has passed, when neural activity is suppressed.
Improvements to the method could include continuous scanning (pre- and during aura), however, this is difficult to implement. This work brings us a step closer to characterizing the uncharted terrain of migraine aura, beyond descriptive symptoms and towards an empirically devised disease prognosis.



