In a Best-in-Physics presentation at the AAPM Annual Meeting, Eric Diffenderfer compared four FLASH proton delivery techniques from a radiophysical, radiochemical and radiobiological perspective

FLASH radiotherapy – the delivery of therapeutic radiation at ultrahigh dose rates – offers the potential to vastly reduce normal tissue toxicity while maintaining anti-tumour activity. While almost all studies to date have been pre-clinical, the first patient treatment with FLASH was performed at Lausanne University Hospital in 2019, and the first clinical trial in humans completed accrual last year.
Most pre-clinical FLASH studies, as well as the patient treatment, used electrons. But proton therapy systems can also deliver FLASH dose rates, and could prove particularly promising for clinical use, offering more conformal dose distribution than electrons and the ability to treat deeper tumours. Proton beams can be delivered using various techniques that create distinct spatial-temporal dose-rate structures. So which is the most optimal modality for delivering FLASH proton beams?

A team led by Eric Diffenderfer from the University of Pennsylvania is using computational modelling to find out. Diffenderfer (presenting on behalf of first author Ray Yang from BC Cancer) described the group’s work to quantitatively determine which aspects of the proton dose-rate structure maximize the FLASH effect.
The researchers simulated four modes of proton FLASH delivery: pencil-beam scanning (PBS), which provides the highest instantaneous focal dose rate; double-scattering using a ridge filter; range-modulated double-scattering using a rotating modulator wheel; and a hybrid PBS-RF approach in which the pencil beam is delivered through a ridge filter to irradiate all depths simultaneously.
They then compared the impact of these different FLASH delivery modes on normal tissue sparing. In particular, they examined three surrogate metrics of tissue sparing: the oxygen depletion effect; kinetics of organic radical species formation; and survival of circulating immune cells.
To model these metrics, each technique was used to deliver a spatially equivalent spread-out Bragg peak plan with 11 energy layers to a 5x5x5 cm target. The cyclotron output for FLASH was defined as a beam current of 500 nA, which gives a dose rate of approximately 2 Gy/ms at the Bragg peak.
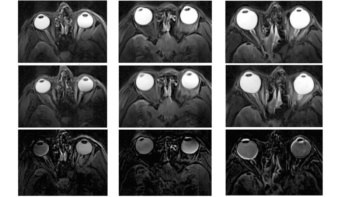
The model calculates spatial dose distributions using machine data from the IBA proton therapy system at Penn. The team then used the model outputs to quantify the abovementioned radiophysical, radiochemical and radiobiological parameters, on a voxel-by-voxel basis. Diffenderfer noted that the model’s flexibility enables parameters to be refined for comparison with new experimental evidence.
The researchers first examined radiosensitivity modulation via the oxygen effect: the hypothesis that oxygen depletion at ultrahigh dose rates mimics hypoxia in normal tissues, making them more radioresistant. Diffenderfer showed how at ultrahigh dose rates, transient oxygen depletion occurs differentially over space and time and reduces the effective dose deposition.
The team calculated the dose rate-dependent oxygen depletion and recovery, and determined energy deposition versus oxygen concentration for all four delivery modes. The hybrid PBS-RF technique exhibited the most significant downward shift in oxygen concentration.
Oxygen is just one of several dose rate-dependent species that facilitate the formation of organic radicals, a known precursor to DNA damage. So next, the researchers used radiochemical rate equations to determine the concentration of organic radicals over time, with the cumulative area under the curve a surrogate metric for DNA damage. For all four delivery methods, FLASH reduced the level of damage compared with the corresponding conventional irradiation.
Another potential mechanism proposed to explain FLASH’s tissue-sparing effect is the reduction in radiation-induced death of circulating immune cells at ultrahigh dose rates. To investigate this, the team implemented a radiobiological model that considers how radiation intersects with the circulating blood pool to quantify the survival of immune cells.
Plotting the proportion of immune cells killed as function of dose rate for the four techniques revealed that PBS causes the greatest cell death, likely because it allows the most time for different parts of the blood pool to be exposed to radiation.
Could proton FLASH prove optimal for clinical application?
Overall, all three mechanistic models agreed on their rankings, with the most tissue sparing seen for the PBS-RF model. The least effective delivery techniques was PBS, likely due to its inherent long slew times (particularly for energy-layer switching) allowing significant oxygen replenishment, increased retention of radicals and reduced immune cell survival.
“We identified differences in spatial-temporal dose-rate structure for different delivery techniques and how that influences tissue sparing at ultrahigh dose rates, in a more subtle way than just looking at the field-averaged dose rate,” Diffenderfer concluded. The team’s findings could pave the way to better understanding and adapting the spatial-temporal structure of proton treatment plans to maximize the FLASH effect.