Malaria remains a serious health concern, with annual deaths increasing yearly since 2019 and almost half of the world’s population at risk of infection. Existing diagnostic tests are less than optimal and all rely on obtaining an invasive blood sample. Now, a research collaboration from USA and Cameroon has demonstrated a device that can non-invasively detect this potentially deadly infection without requiring a single drop of blood.
Currently, malaria is diagnosed using optical microscopy or antigen-based rapid diagnostic tests, but both methods have low sensitivity. Polymerase chain reaction (PCR) tests are more sensitive, but still require blood sampling. The new platform – Cytophone – uses photoacoustic flow cytometry (PAFC) to rapidly identify malaria-infected red blood cells via a small probe placed on the back of the hand.
PAFC works by delivering low-energy laser pulses through the skin into a blood vessel and recording the thermoacoustic signals generated by absorbers in circulating blood. Cytophone, invented by Vladimir Zharov from the University of Arkansas for Medical Science, was originally developed as a universal diagnostic platform and first tested clinically for detection of cancerous melanoma cells.
“We selected melanoma because of the possibility of performing label-free detection of circulating cells using melanin as an endogenous biomarker,” explains Zharov. “This avoids the need for in vivo labelling by injecting contrast agents into blood.” For malaria diagnosis, Cytophone detects haemozoin, an iron crystal that accumulates in red blood cells infected with malaria parasites. These haemozoin biocrystals have unique magnetic and optical properties, making them a potential diagnostic target.

“The similarity between melanin and haemozoin biomarkers, especially the high photoacoustic contrast above the blood background, motivated us to bring a label-free malaria test with no blood drawing to malaria-endemic areas,” Zharov tells Physics World. “To build a clinical prototype for the Cameroon study we used a similar platform and just selected a smaller laser to make the device more portable.”
The Cytophone prototype uses a 1064 nm laser with a linear beam shape and a high pulse rate to interrogate fast moving blood cells within blood vessels. Haemozoin nanocrystals in infected red blood cells absorb this light (more strongly than haemoglobin in normal red blood cells), heat up and expand, generating acoustic waves. These signals are detected by an array of 16 tiny ultrasound transducers in acoustic contact with the skin. The transducers have focal volumes oriented in a line across the vessel, which increases sensitivity and resolution, and simplifies probe navigation.
In vivo testing
Zharov and collaborators – also from Yale School of Public Health and the University of Yaoundé I – tested the Cytophone in 30 Cameroonian adults diagnosed with uncomplicated malaria. They used data from 10 patients to optimize device performance and assess safety. They then performed a longitudinal study in the other 20 patients, who attended four or five times at up to 37 days following antimalarial therapy, contributing 94 visits in total.
Photoacoustic waveforms and traces from infected blood cells have a particular shape and duration, and a different time delay to that of background skin signals. The team used these features to optimize signal processing algorithms with appropriate averaging, filtration and gating to identify true signals arising from infected red blood cells. As the study subjects all had dark skin with high melanin content, this time-resolved detection also helped to avoid interference from skin melanin.
On visit 1 (the day of diagnosis), 19/20 patients had detectable photoacoustic signals. Following treatment, these signals consistently decreased with each visit. Cytophone-positive samples exhibited median photoacoustic peak rates of 1.73, 1.63, 1.18 and 0.74 peaks/min on visits 1–4, respectively. One participant had a positive signal on visit 5 (day 30). The results confirm that Cytophone is sensitive enough to detect low levels of parasites in infected blood.
The researchers note that Cytophone detected the most common and deadliest species of malaria parasite, as well as one infection by a less common species and two mixed infections. “That was a really exciting proof-of-concept with the first generation of this platform,” says co-lead author Sunil Parikh in a press statement. “I think one key part of the next phase is going to involve demonstrating whether or not the device can detect and distinguish between species.”

Performance comparison
Compared with invasive microscopy-based detection, Cytophone demonstrated 95% sensitivity at the first visit and 90% sensitivity during the follow-up period, with 69% specificity and an area under the ROC curve of 0.84, suggesting excellent diagnostic performance. Cytophone also approached the diagnostic performance of standard PCR tests, with scope for further improvement.
Staff required just 4–6 h of training to operate Cytophone, plus a few days experience to achieve optimal probe placement. And with minimal consumables required and the increasing affordability of lasers, the researchers estimate that the cost per malaria diagnosis will be low. The study also confirmed that the safety of the Cytophone device. “Cytophone has the potential to be a breakthrough device allowing for non-invasive, rapid, label-free and safe in vivo diagnosis of malaria,” they conclude.

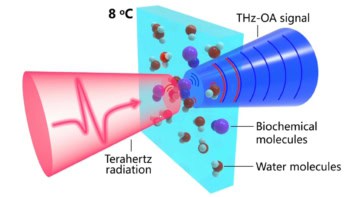
Portable magneto-optical device can detect malaria rapidly
The researchers are now performing further malaria-related clinical studies focusing on asymptomatic individuals and children (for whom the needle-free aspect is particularly important). Simultaneously, they are continuing melanoma trials to detect early-stage disease and investigating the use of Cytophone to detect circulating blood clots in stroke patients.
“We are integrating multiple innovations to further enhance Cytophone’s sensitivity and specificity,” says Zharov. “We are also developing a cost-effective wearable Cytophone for continuous monitoring of disease progression and early warning of the risk of deadly disease.”
The study is described in Nature Communications.