New ultralow-field MRI scanners are bringing unprecedented flexibility at low cost to the clinical setting, registrants heard at ECR 2021. Presenting the benefits of ultralow-field MRI, Mathieu Sarracanie, co-head of the Adaptable MRI technology (AMT) Center at the University of Basel, Switzerland, said both the upper and lower ends of the ultralow-field spectrum that feature in two recently-launched devices will shine bright in the modality’s future.
The lower end and the higher end of low-field MRI, bring benefits and value, including performance, lower costs, and easier siting than 1.5-tesla (T) and 3T MRI, he noted, including the unfriendly environment of the intensive care unit (ICU). However, within the range of low-field, advantages may vary.
Illustrating the differences between ultralow-field scanners, he cited two commercial systems as case examples. The Siemens Magnetom Free.Max, a 0.55T scanner with an 80-cm bore, weighs in at 3.2 metric tons (3200 kg). This scanner has been used routinely for imaging the abdomen, as well as for different organs such as the lungs and for cardiovascular procedures.

“The major pro is that it is basically a standard MRI, it has a large bore, no quench line, which is a huge advantage, no need for helium refill and shows very good imaging performance. The cons are (also) that it is basically a standard MRI, and the siting is similar to a 1.5T machine,” noted Sarracanie, pointing out that this solution might not be suitable for ICU, and that it might be problematic for neurological applications where resolution and the capacity to leverage susceptibility contrast are key.
Sarracanie pointed to the Hyperfine scanner as his second example, noting that he co-founded the ultralow-field MRI startup in 2014 with the aim of bringing MRI to places where previously it wasn’t feasible.
The Hyperfine SWOOP, a 64mT machine, intended mostly for head injury but also MSK wrist, knee and foot imaging, can be located in smaller and more crowded spaces such as the ICU, stroke unit, outpatient centres, and paediatric departments. The average scan for a patient is 35 minutes and that includes T1, T2, FLAIR, and diffusion imaging with 3D slices and millimetric resolution, he said. The Hyperfine needs a monthly subscription and has to be integrated into the hospital’s PACS.

“This solution is truly disruptive, in the sense that the technology allows for a paradigm change. It has a small footprint and is also mobile. These machines don’t need any specific siting and the cost is low. The con is that these devices are purpose-built and some customers may see that as a disadvantage,” Sarracanie said.
Pointing to Hyperfine’s imaging capacity, he noted that grey- and white-matter contrast can show very high dispersion at lower field strength. This has been explored by the researchers at the University of Aberdeen, UK, who have generated some fascinating T1 contrast results in stroke patients thanks to a novel fast-field cycling MR scanner, he noted.
“Now is the time for ultralow-field MRI. The 0.55T machine could be a serious contender to the standard 1.5T as it is more compact and cost-efficient. Machines at even lower field strength will not replace MRI as we know it but will expand its use and bring it to other places that we don’t know yet,” Sarracanie added.
7T detail
High-field MRI of 7T and above might seem like a cool toy with little clinical benefit, but in October 2017, the FDA approved the first 7T MRI platform for clinical use, pushing it from the realm of research to the clinical world, according to Anja van der Kolk, a neuroradiologist at the UMC Utrecht and Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital in Amsterdam, who spoke about the benefits of ultrahigh-field MRI in brain diseases during the same ECR session, organized jointly by the European Society of Radiology and European Federation of Organisations for Medical Physics.

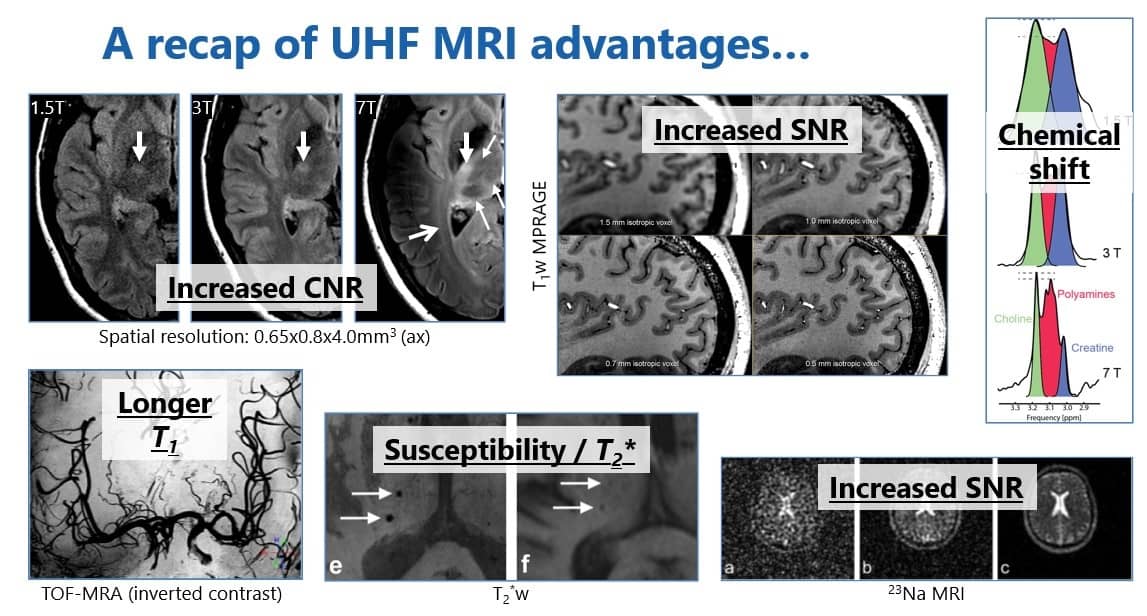
Ultrahigh-field MRI provides more anatomical detail due to higher spatial resolution within a reasonable scan time. New detail can be gleaned from T2-weighted imaging because of the increased susceptibility effects. Increased signal-to-noise ratio also enables metabolic imaging and imaging of x-nuclei, while increased spectral resolution makes it possible to distinguish metabolic peaks that overlap on 1.5T.
Now essential for certain areas of healthcare, the advantages of ultrahigh-field translate not only into direct clinical benefits such as diagnosis, treatment and prognosis of disease, but also indirect ones such as knowledge about the development of diseases, their associated factors, and the effects of these diseases on other organ systems.
“These indirect benefits have a significant impact on our understanding of diseases and how to potentially diagnose and treat them in a better way,” she said.
Novel techniques
One of high-field MRI’s most promising applications is metabolic imaging, such as MR spectroscopy, chemical exchange saturation transfer, and sodium and x-nuclei MRI, according to van der Kolk.
“Specifically, in sodium MRI of brain tumours you can see high sodium concentration inside the enhancing part of the tumour, but also within the T2 hyperintense area around the tumour and which we know is caused by oedema and tumour cells. This may be a way to visualize infiltrative tumour cells,” she noted.
But should radiologists view ultrahigh-field MRI as a specialized platform for only some rare or difficult cases or as a routine platform and part of the MRI workforce?
Van der Kolk’s view falls between the two extremes. At the moment a specialized platform for specific cases, this niche modality may be used more routinely with time.
“Future studies will show if it is going to become the next 3T scanner,” she noted.
Clinical use
Her talk covered several specific neurological diseases already benefitting from ultrahigh-field MRI such as MRI-negative/cryptogenic epilepsy, Parkinson’s disease, deep-brain stimulation, multiple sclerosis, pituitary (micro)adenomas and brain tumours.
Ultrahigh-field MRI can have a clinical benefit in epilepsy, and this is because 30% of patients with the condition have the cryptogenic type, meaning no anatomical focus can be found. However, 7T MRI can detect new lesions that cannot be detected at lower field strengths in 30% to 40% of patients. Lesions such as focal cortical dysplasia, polymicrogyria, and mesial temporal sclerosis can be missed on 3T. And while these lesions can be seen on 3T retrospectively, she noted that the 3T images that illustrated her cases were performed in centres where dedicated epilepsy radiologists with high experience in detecting these abnormalities had missed them on 3T and had only seen them retrospectively on the original images once detected on 7T.
In addition to more accurate detection of the causes of epilepsy, and better assessment of Parkinson’s disease, the targeting of deep-brain stimulation electrodes also can be optimized through improved visualization of the basal ganglia and other grey-matter structures. Ideally, these electrodes should be localized in the dorsal border of the subthalamic nucleus – more readily visualized on 7T than on other field strengths.
Proven advantages
Multiple sclerosis is one of the best-studied diseases with 7T, and it leads to better lesion detection in younger patients for earlier diagnosis, as well as differentiation from other white-matter lesions: ultrahigh-field MRI was the first technique to depict the small central vein sign, which is characteristic of multiple sclerosis lesions and not seen in other white matter hyperintensities, van der Kolk noted. Also, it depicts paramagnetic phase changes and a persistent hypointense rim that can predict outcome in these patients.
She also pointed to 7T’s improved detection of very small microadenomas which would otherwise be missed on lower field strengths, making presurgical planning difficult.
Meanwhile for brain tumours, using 7T’s increased susceptibility effects and spectral resolution doctors can detect the 2-hydroxyglutarate peak, specific to gliomas, for example, while tumour progression is shown using the susceptibility effects of microvascularity, which increases during treatment.
However, there are challenges, she said. So far it is unclear what the clinical consequences of some findings will be, and importantly nonradiology clinicians will have to know what the advantages of ultrahigh-field scans are in order to request them.
- This article was originally published on AuntMinnieEurope.com ©2021 by AuntMinnieEurope.com. Any copying, republication or redistribution of AuntMinnieEurope.com content is expressly prohibited without the prior written consent of AuntMinnieEurope.com.