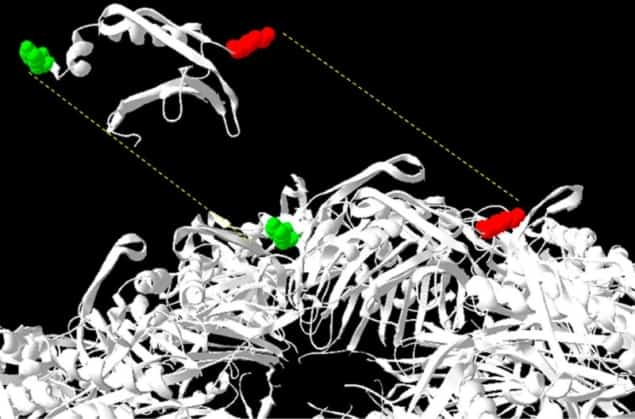
Qb virus-like particles (VLPs) are small nanoparticles that can be used to deliver drugs to the human body. Natural Qb VLPs form from 180 copies of the coat protein – self-assembling proteins that viruses produce to encapsulate and protect their genetic material. Researchers at Occidental College engineered hybrid VLPs by co-expressing normal coat proteins and coat proteins fused to peptides that bind heparin, a widely used blood-thinner. The assembled nanoparticles, containing up to 31% peptide-fused coat protein, effectively hindered heparin activity in a laboratory-based clotting assay (Mol. Pharmaceutics 10.1021/acs.molpharmaceut.8b00135).
Controlling blood clotting
Heparin is a natural molecule that is the most commonly used anticoagulant, or blood-thinner. It is an extremely important medication, even included on the WHO Essential Medicines List, and is used to prevent blood clots. However, too much heparin can cause uncontrolled bleeding and lead to death.
The only current available drug for reversing heparin activity is a mixture of peptides (very small proteins composed of fewer than 50 amino acids) called protamine. Protamine can, however, cause severe side-effects when administered in humans, which makes finding other therapies with reduced toxicity an important clinical goal.
Anti-heparin nanoparticles
Justin Choi and a team of researchers from Andrew Udit’s laboratory have found an alternate way of stopping heparin activity. Previous research showed that different cationic peptides (peptides with a positive charge) interact with heparin. This led Choi’s team to hypothesize that the effectiveness of these peptides will increase when combined in greater number on a nanoparticle. The scientists also hypothesized that conjugation could reduce the toxicity of the peptides.
To test this hypothesis, the research team fused many different peptides onto Qb coat proteins and assembled the particles by expressing these coat proteins alongside unmodified coat proteins. The peptides that they tested all had the sequence XBBBXBX, where B was a basic amino acid and X was a hydrophobic amino acid.
The generated hybrid particles had different amounts of peptide displayed on their surface, ranging from 8-31%.
Determining nanoparticle effectiveness
Heparin works by activating antithrombin, a protein that inactivates enzymes in the human blood that cause it to clot. To measure heparin and heparin-inactivating drug activity, scientists use a laboratory-based test called the activated partial thromboplastin time (APTT) assay, which measures the overall speed at which blood clots.
The California researchers saw that normal blood-clotting in the assay took 37 s, whereas blood clotting was hindered when heparin was present. The addition of conjugated Qb VLPs to samples containing heparin restored blood-clotting to almost normal times. The effectiveness of the particles varied, with the best particle being the one with the greatest amount (31%) of incorporated peptide. They note that the peptides benefit from being conjugated onto a VLP – the same amount of unconjugated peptide did not fully antagonize heparin activity in the assay.
The future of nanoparticles
The research presented by Andrew Udit’s team shows that conjugating heparin blockers to VLPs improves their activity. This is highly important since less concentrated therapeutic doses of peptides means less toxicity to the human system. Exciting avenues for future exploration include optimizing the peptide sequences even further and creating particles with higher conjugation. In general, the field of VLPs and nanoparticles is growing fast, with recent advances in drug delivery, targeting of drug-resistant tumours and even as vaccines against Alzheimer’s disease.



