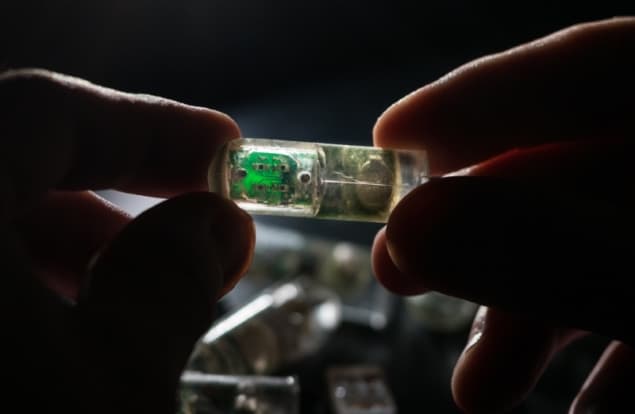
MIT researchers have built an ingestible sensor equipped with genetically engineered bacteria that can diagnose bleeding in the stomach or other gastrointestinal (GI) problems. The prototype device, dubbed IMBED (ingestible micro-bio-electronic device), could eventually be rendered small enough for a human patient to ingest, enabling physicians to better manage or diagnose a range of gut-related diseases (Science 360 915).
The IMBED features bacterial cells designed to sense disease biomarkers, placed in individual wells covered by a semipermeable membrane. When target molecules diffuse across the membrane they activate the bacteria, causing them to generate light. This light is detected by photodetectors underneath each well, and the resulting electrical signals are transmitted wirelessly to an external radio or mobile phone.
“By combining engineered biological sensors together with low-power wireless electronics, we can detect biological signals in the body in near real-time, enabling new diagnostic capabilities for human health applications,” said MIT’s Timothy Lu.
As an initial proof-of-concept, the team developed a version of IMBED that detects bleeding in the GI tract. They engineered a probiotic strain of E. coli to express a genetic circuit that causes the bacteria to emit light when they encounter haem, and placed the bacteria into four wells on the sensor.
The sensor, which is a cylinder about 3.8 cm long, requires about 13 µW of power, enabling a 2.7 V battery to power the device for about 1.5 months. It could also be powered by a voltaic cell sustained by acidic fluids in the stomach, using technology that the team previously developed.
The researchers tested the IMBED in pigs and showed that it could correctly determine whether any blood was present in the stomach. They anticipate that this type of sensor could be deployed for one-time use or remain the digestive tract for several days or weeks, sending continuous signals. To help move toward patient use, the researchers plan to reduce the sensor size and to study how long the bacteria cells can survive in the digestive tract.
In addition to blood sensing, the researchers adapted the IMBEDs to sense two other molecules: thiosulfate and acyl-homoserine lactone (AHL). Thiosulfate is linked to inflammation and could be used to monitor patients with Crohn’s disease, for example, while AHL can serve as a marker for gastrointestinal infections.
“Most of the work we did in the paper was related to blood, but conceivably you could engineer bacteria to sense anything and produce light in response to that,” explained co-lead author Mark Mimee. “Anyone who is trying to engineer bacteria to sense a molecule related to disease could slot it into one of those wells, and it would be ready to go.”
The sensors could also be designed to carry multiple strains of bacteria, allowing them to diagnose a variety of conditions. “Right now, we have four detection sites, but if you could extend it to 16 or 256, then you could have multiple different types of cells and be able to read them all out in parallel,” said co-lead author Phillip Nadeau.