A team of researchers from Stanford University has developed a promising hydrogel formulation and demonstrated how it could provide a valuable tool for the delivery of multiple drugs in vivo to treat complex diseases (Advanced Healthcare Materials 10.1002/adhm.201801147).
Hydrogels represent one of the current frontiers in tissue engineering and regenerative medicine, due to their biocompatibility and physiologically-relevant properties. During the last few decades, numerous advances in the field led to the development of a variety of hydrogel formulations capable of delivering drugs and cells directly to the site of injury in various tissue types.
The application of hydrogel scaffolds to the clinic is currently hindered by two major hurdles: scalability and the invasive nature of delivery techniques. Injectable hydrogels represent an innovative way to reduce the invasiveness of in vivo delivery. However, currently available injectable hydrogels fail to combine functionality, biocompatibility and scalability, mainly due to extensive synthesis protocols and/or complex formulations.
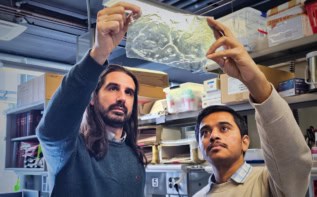
The hydrogel developed by the Stanford team overcomes such limitations, being both biocompatible and easy and quick to produce. The major breakthrough, however, is the technique through which the hydrogel is delivered: it can be quickly and effortlessly injected through a long and thin clinical catheter. Most importantly, the transiently “broken” gel readily recovers its original structure immediately after injection, overcoming the limitations of current hydrogels.
The researchers achieved these characteristics through the combined use of high molecular weight hyaluronic acid (HA), a polymer that is widely distributed in the human body, and poly(ethylene glycol)‐block‐poly(lactic acid) nanoparticles. The functionalization of HA with long hydrophobic moieties allowed for a strong, but reversible, interaction between the two components of the hydrogel. This enabled the transient loss of stiffness upon pressure during injection, and the subsequent quick gelation once the viscous solution reached the other side of the catheter.
Moreover, the authors demonstrated that the characteristic, beneficial effects of HA (cell survival, proliferation and migration) were maintained by the polymer in the formulation. They also showed the hydrogel’s robust haemocompatibility and biocompatibility in vivo in rat models.
Incorporation of a blood vessel growth-promoting molecule, ESA, into the hydrogel resulted in the sustained release of this functional molecule over time. Interestingly, the researchers found that incorporating ESA into the nanoparticles markedly prolonged its release rate, suggesting the possibility for the hydrogel to be employed as a tool for administering complex therapies.
“In future studies, we plan to investigate this hydrogel as a minimally-invasive delivery vehicle of growth factors and cells to treat myocardial infarction,” says first author Amanda Steele. The authors add that their future work will also focus on the loading of more than one therapeutic molecule into the gel. Considering the different release rates of the two phases of the hydrogel, their efforts could provide a valuable tool for in vivo delivery of different molecules at programmed times.