Radiation exposure to the hippocampus during whole-brain radiotherapy is associated with cognitive decline. As such, hippocampal irradiation should be minimized at the treatment planning stage. Intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT) are both able to reduce radiation dose to hippocampi. Radiation oncologists at Mayo Clinic hypothesized that intensity-modulated proton therapy (IMPT) — with its capability to modulate both proximal and intermediate doses and provide distal target conformity — could deliver even less dose.
The team has now conducted a study to determine the radiation dose-sparing benefits of IMPT compared with VMAT, for both adult and paediatric patients (Phys. Imag. Radiat. Oncol. 10.1016/j.phro.2018.11.001).
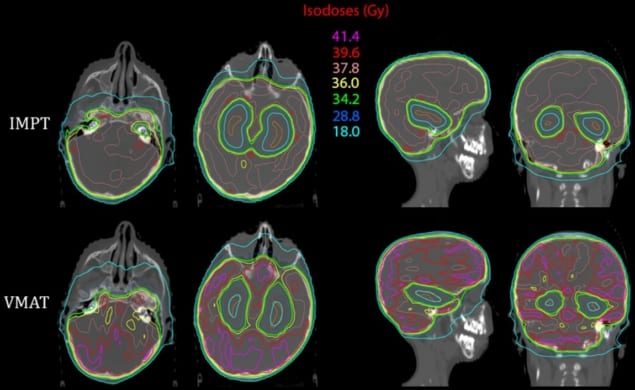
Lead author Joshua Stoker and colleagues created VMAT and IMPT treatment plans for 10 adult and 10 paediatric patients who had been previously treated with X-ray therapy at Mayo Clinic Arizona, the majority for central nervous system (CNS) malignancies. IMPT systems utilize individual beamlets that have optimized intensities to provide a balance between target dose and dose to normal tissues. They offer improved efficiency, proximal dose sparing and flexible applications compared with legacy double-scattering proton delivery systems.
The researchers delineated target structures and organs-at-risk (OAR), and contoured the hippocampus around the grey matter signal in the medial temporal lobe. They defined the clinical target volume (CTV) as the brain, including meninges, but excluding the hippocampi. Treatment plans for adults specified a 30 GyE (radiobiological gray equivalent) dose to be delivered in 10 fractions to 95% of the CTV; the paediatric plans specified 36 GyE in 20 fractions. The CTV was identical for the IMPT and VMAT plans to validate dosimetric comparison.
The authors recorded the volumes of total CTV receiving at least 95% of the prescribed dose, and also evaluated the mean, maximum and minimum doses for hippocampi, cochlea and lenses. They found that IMPT maintained CTV coverage but reduced the homogeneity index by roughly half.
For adults, the mean dose to both hippocampi was reduced from 11.7 Gy with VMAT to 4.4 GyE with IMPT. For paediatric patients, IMPT reduced the mean doses from 13.7 Gy to 5.4 GyE. IMPT also reduced dose to the lenses and to the cochlea, by approximately 50% and 15–18%, respectively.
The authors caution, however, that the hippocampi must be accurately delineated to achieve these outcomes, and that this process can be difficult for some clinicians.
The researchers point out that while IMPT could potentially benefit any patient receiving radiotherapy for malignant brain tumours, paediatric patients and patients with primary CNS malignancies (who have superior survival expectations compared with patients with metastatic disease) might receive the greatest benefit.
“The cognitive and quality-of-life benefits of hippocampal avoidance IMPT in paediatric patients could be substantial,” they wrote. “This increased dosimetric benefit to OAR may warrant inclusion of the IMPT modality as part of any upcoming clinical investigations into hippocampal avoidance for paediatric populations.”



