Recent advances in scanner technology have made the use of CT stress myocardial perfusion imaging feasible. Just how well it matches up to MR perfusion in the diagnosis of coronary artery disease (CAD) is the central question of a German/US study led by Marc Dewey from Berlin.
Senior author Dewey collaborated with colleagues from various healthcare institutions to investigate the diagnostic performance of CT perfusion and MR perfusion in patients suspected of having CAD at the US National Institutes of Health (NIH) and Charité-Universitätsmedizin Berlin in Germany. They found that CT and MR perfusion had similar accuracies in detecting CAD, and that either imaging modality was suitable for evaluating the functional relevance of coronary stenosis.
“The results of this study provide reassurance that clinicians have two viable options in assessing the functional significance of coronary artery disease,” said co-first author Marcus Chen. “The decision regarding which test to select may be institutional and clinician-dependent or vary depending upon regional reimbursement patterns.”
Comprehensive coronary assessment
To accurately diagnose and comprehensively assess coronary artery disease, it is important to evaluate the heart both anatomically and physiologically, i.e., how well it functions. The gold standard for this process has been invasive coronary angiography (ICA) combined with fractional flow reserve (FFR) measurements. But clinicians have been leaning toward different, noninvasive means of detecting obstructive CAD, not only because noninvasive imaging tests can improve clinical outcomes, but also because they save economic resources, according to the researchers (Radiology 286 461).
Coronary CT angiography is one of the most popular noninvasive methods to spot the presence of CAD due to its high diagnostic yield and capacity to shorten hospital stays. And for the functional assessment of CAD, one of the most common noninvasive techniques is myocardial perfusion imaging via SPECT or MR perfusion. With recent technological advancements to CT scanners – such as shortened scanning time, increased area of coverage, and improved temporal and spatial resolution – CT perfusion has also become a viable option.
“A convenient advantage of CT perfusion imaging is given by the fact that it can be performed immediately after CT coronary angiography in the same scan setting, and that no further imaging modality needs to be included,” said co-first author Matthias Rief. “This may also be particularly preferable for the patient, as only one appointment is necessary.”
Yet the viability of CT perfusion in clinical practice is still in question. The medical community is particularly at odds over its use due to safety concerns stemming from radiation exposure.
Though the technique only increases the radiation dose by about 50%, that dose is restricted to a much smaller volume of tissue, thus accentuating the potential harm it could cause, the authors noted. Other techniques such as MR perfusion can determine whether or not a coronary stenosis causes myocardial ischemia without exposing patients to radiation.
Comparable diagnostic accuracy
Seeking to address these concerns with CT perfusion, the researchers compared its ability to that of MR perfusion in diagnosing obstructive CAD in a substudy of the Combined Noninvasive Coronary Angiography and Myocardial Perfusion Imaging Using 320-Detector Computed Tomography (CORE320) multicentre trial.
For the prospective sub study, 92 patients each underwent four imaging exams: invasive coronary angiography with quantitative coronary analysis (QCA), SPECT, CT perfusion (Aquilion One, Canon Medical) and MR perfusion (Magnetom Avanto or Magnetom Sonata, Siemens Healthineers). The median effective radiation dose for the patients was 5.3 mSv for CT perfusion and 19.6 mSv for combined angiography and SPECT.
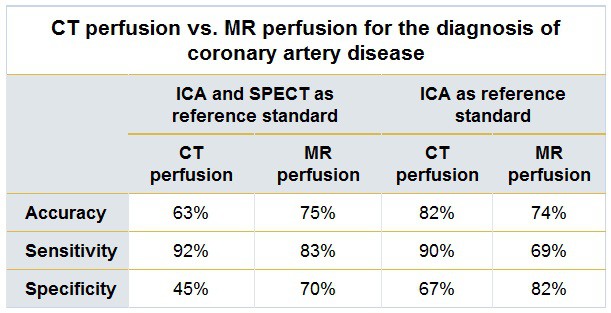
Overall, CT perfusion and MR perfusion displayed comparable diagnostic performance in the detection of CAD when compared with either the primary reference standard of ICA and SPECT (p = 0.11) or the secondary reference standard of ICA alone (p = 0.27).
“With a comparable diagnostic performance, CT and MR perfusion imaging seem to be equally suited for decision-making about the functional relevance of coronary artery stenosis and act as an alternative to SPECT,” said co-author Patricia Bandettini.
Though the differences in accuracy between CT perfusion and MR perfusion were not statistically significant, there were significant differences for sensitivity and specificity. CT perfusion had a higher sensitivity than MR perfusion based on the secondary reference standard (p < 0.01), but a lower specificity than MR using the primary reference standard (p < 0.01).
The higher sensitivity of CT perfusion may be a result of its enhanced spatial resolution, and its lower specificity might be tied to its susceptibility to beam-hardening artefacts, which can look like perfusion defects, he said.
Promising performance
Though the study included one of the largest cohorts of patients who underwent myocardial perfusion imaging through multiple modalities, it still had a limited patient population from the two sites, the investigators said. The study also demonstrated the wide variability in CAD detection when referring to different standards. The group reported a coronary artery stenosis with 50% or more obstruction in 64% of the patients using invasive angiography alone, but in only 39% of patients after combining ICA with SPECT.
“This [variation] shows one of the major challenges of modern cardiac and coronary imaging, whereby, depending on the reference standard, different results may occur and higher stenosis degrees do not necessarily cause more corresponding perfusion defects,” Rief said.
So far, the results suggest that the complementary and necessary information to identify culprit coronary artery lesions is available through both CT perfusion and MR perfusion imaging, he said. But whether or not performing coronary CT angiography and CT perfusion in an all-inclusive exam is sufficiently effective to warrant its elevated radiation dose will require further investigation.

To what extent clinicians can use CT perfusion to guide patient care decisions – like with FFR – is a pivotal clinical question emerging from this study, according to the authors. They recommend continuing research in the form of randomized trials to establish a more definitive answer.
- This article was originally published on AuntMinnieEurope.com.
© 2018 by AuntMinnieEurope.com. Any copying, republication or redistribution of AuntMinnieEurope.com content is expressly prohibited without the prior written consent of AuntMinnieEurope.com.