
A team of scientists based in the US has developed a non-invasive headset device designed to track changes in blood flow and assess a patient’s stroke risk. The device could make it easier to detect early signs of stroke, offering patients and physicians a direct, cost-effective approach to stroke prevention.
The challenge of stroke risk assessment
Stroke remains the leading cause of death and long-term disability, affecting 15 million people worldwide every year. In the United States, someone dies from a stroke roughly every 3 min. Those who survive are often left physically and cognitively impaired.
About 80% of strokes occur when a blood clot blocks an artery that carries blood to the brain (ischaemic stroke). In other cases, a blood vessel can rupture and bleed into the brain (haemorrhagic stroke). In both types of stroke, deprived of oxygen from the loss of blood flow, millions of brain cells rapidly die every minute, causing devastating disability and even death.
As debilitating as stroke is, current methods for assessing stroke risk remain limited. Physicians typically use a questionnaire that assesses factors such as demographics, blood test results and pre-existing medical conditions to estimate a patient’s risk. While non-invasive techniques exist to detect changes after the onset of a stroke, by the time a stroke is suspected and patients are rushed to the emergency room, critical damage may have already been done.
Consequently, there remains an acute need for tools that can proactively monitor and quantify stroke risk before an event occurs.
Blood flow dynamics as proxies for stroke risk
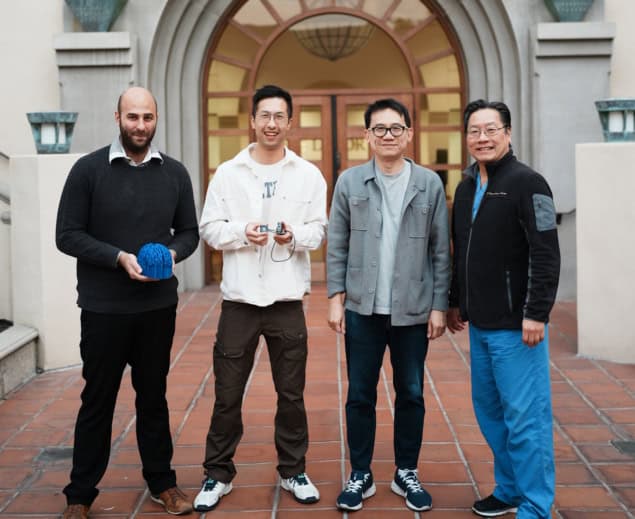
Seeking to bridge this gap, in a study published in Biomedical Optics Express, a research team, led by Charles Liu of the Keck School of Medicine at the University of Southern California and Changhuei Yang of California Institute of Technology, developed a headset device to monitor changes in the brain’s blood flow and volume while a patient holds their breath.
“Stroke is essentially a brain attack. The stroke world has been trying to draw a parallel between a heart attack and a brain attack,” explains Liu. “When you have a heart disease, under normal circumstances – like sitting on the couch or walking to the kitchen – your heart may seem fine. But if you start walking uphill, you might experience chest pain. For heart diseases, we have the cardiac stress test. During this test, a doctor puts you on a treadmill and monitors your heart with EKG leads. For stroke, we do not have a scalable and practical equivalent to a cardiac stress test.”
Indeed, breath holding temporarily stresses the brain, similar to the way that walking uphill or running on a treadmill would stress the heart in a cardiac stress test. During breath holding, blood volume and blood flow increase in response to lower oxygen and higher carbon dioxide levels. In turn, blood vessels dilate to mitigate the pressure of this increase in blood flow. In patients with higher stroke risk, less flexible blood vessels would impede dilation, causing distinct changes in blood flow dynamics.
Researchers have long had access to various imaging techniques to measure blood dynamics in the brain. However, these methods are often expensive, invasive and impractical for routine screening. To circumvent these limitations, the team built a device comprising a laser diode and a camera that can be placed on the head with no external optical elements, making it lightweight, portable, and cost-effective.
The device transmits infrared light through the skull and brain. A camera positioned elsewhere on the head captures the transmitted light through the skull. By tracking how much the light intensity decreases as it travels through the skull and into the camera, the device can measure changes in blood volume.
When a coherent light source such as a laser scatters off a moving sample (i.e., flowing blood), it creates a type of granular interference pattern, known as a speckle pattern. These patterns fluctuate as blood moves through the brain – the faster the blood flow, the quicker the fluctuations. This technique, called speckle contrast optical spectroscopy (SCOS), enables the researchers to non-invasively measure the blood flow rate in the brain.
The researchers tested the device on 50 participants, divided into low- and high-risk groups based on a standard stroke-risk calculator. During a breath-holding exercise, they found significant differences in blood dynamic changes between people with high stroke risk and those at lower risk.
Portable MRI diagnoses stroke at the patient bedside
Specifically, the high-risk group exhibited a faster blood flow rate but a lower volume of blood in response to the brain’s oxygen demands, suggesting restricted blood flow through the stiff vessels. Overall, these findings establish physiological links between stroke risk and blood dynamics measurements, highlighting the technology’s potential for stroke diagnosis and prevention.
The future of stroke prevention
The team plans to expand these studies to a broader population to reinforce the validity of the results. “Our goal is to further develop this concept to ensure it remains portable, compact, and easy to operate without requiring specialized technicians. We believe the design is scalable, aligning well with our vision of accessibility, allowing diverse and underrepresented communities to benefit from this technology,” says co-lead author Simon Mahler, a postdoctoral scholar in the Yang lab at Caltech.
The researchers also aim to integrate machine learning into data analysis and conduct clinical trials in a hospital setting, testing their approach’s effectiveness in stroke prevention. They are also excited about the applications of their device in other neurological conditions, including brain injuries, seizures, and headaches.




