A liquid biopsy simply involves using a patient’s blood from a routine blood draw procedure to diagnose cancer. Although extremely promising as a minimally invasive method to track cancer in patients, the approach has yet to be validated. Researchers at the Cancer Center of Northwestern Universityand Thomas Jefferson University Hospital have retrospectively studied medical records of 91 patients with advanced metastatic breast cancer to demonstrate liquid biopsy as an effective prognostic tool (Clin. Cancer Res. doi: 10.1158/1078-0432.CCR-17-2092).
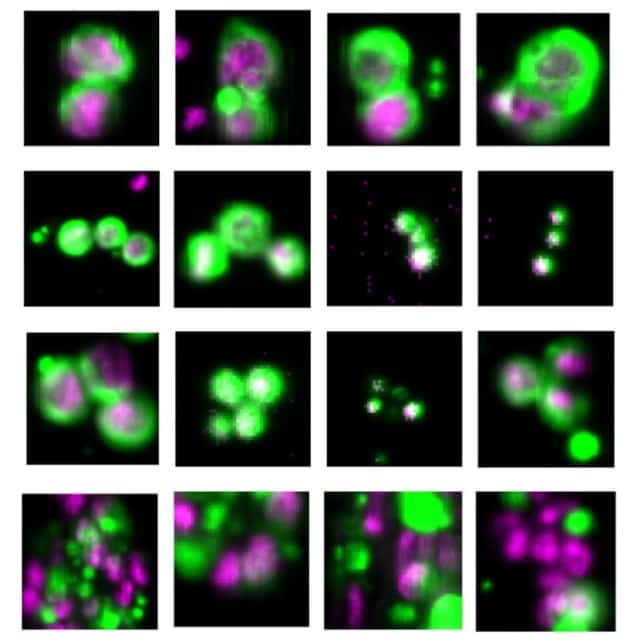
As a tumour grows, it sheds cellular and molecular material that enters the blood circulation. Cancer cells that enter the blood are called circulating tumour cells (CTCs), whereas DNA molecules are referred to as circulating tumour DNA (ctDNA). The research team evaluated increases in CTCs, ctDNA levels, and the number of genetic mutations found in the circulating DNA over a period of three years.

Cancer diagnostics company Guardant Health carried out the blood analysis using Guardant360, a commercially available test that examines more than 50 genes associated with solid tumours. These cancer-related genes are reported in the Catalogue of Somatic Mutations In Cancer (COSMIC), a comprehensive database of cancer-related mutations. In this study, patients’ ctDNA harboured three mutations, on average. The most frequent mutations were found in the cancer-related genes TP53, PIK3CA and ERBB2.
By analysing blood during the first and second years, the research team established threshold levels that could be used as prognostic factors in metastatic breast cancer. As tumour burden increased in patients, not only did the CTCs and ctDNA levels rise, but the number of mutations also rose. The researchers concluded that CTC levels greater than five cells per 7.5 ml of blood, ctDNA greater than 0.5%, and a number of mutations greater than two could be used as prognostic indicators to determine advanced tumour burden in patients.

This prognostic classification is critical in enabling precision medicine, which tailors treatment plans for each individual patient. Such an approach is strongly desirable because genetic mutations related to each individual’s cancer can vary greatly from patient to patient, which leads to variable success rates with systemic treatments. A “one-size-fits-all” does not work for treating all patients. Often, approved targeted therapies are available to use on patients with specific cancer-related mutations. However, if the genetic makeup of the patient’s cancer is unknown, such therapies may not be recommended.
The researchers demonstrated that a comprehensive liquid biopsy analysis provides a useful prognostic tool for assessing tumour burden and genetic features of cancer. These assessments can enable physicians to tailor treatment plans based on the individual needs of the patient.
With minimal invasiveness, the liquid biopsy can pinpoint genetic mutations to target with drugs, monitor response to drugs, and evaluate the benefit of new drugs during the entire course of a patient’s treatment plan. In fact, the authors note that several patients in the study were initiated on targeted therapy based on results of their ctDNA tests.



