In a Best-in-Physics presentation at the AAPM Annual Meeting, Arutselvan Natarajan showed how a long-lived antibody PET tracer could enable biology-guided radiation therapy for five consecutive days following a single tracer injection

Biology-guided radiation therapy (BgRT), in which PET images of the tumour target are used to guide beam delivery, has gained momentum over the last 10–15 years. BgRT, which is currently awaiting approval from the FDA for clinical use, is performed using the positron-emitting PET tracer 18F-FDG. But as Arutselvan Natarajan from Stanford University explained, this may not be the optimal approach.
Natarajan shared an example workflow for a BgRT treatment, pointing out that it typically requires administration of five to seven separate doses of the short-lived 18F-FDG (which has a half-life of about 110 min). “We want to develop an alternative approach, using one injection, a single dose of a long-lived isotope,” he explained. “A long-lived isotope would be very good to track, direct and deliver radiotherapy.”
To achieve this, Natarajan and colleagues combined the positron-emitting isotope 89Zr (which has a half-life of 78 h) with an antibody to create the PET tracer 89Zr-Panitumumab (89Zr-pan). Antibodies are particularly suited to this application as they exhibit high tumour specificity and uptake. Early studies in mice demonstrated that it is possible to track the 89Zr-pan PET signal for nine days following tracer injection.
The researchers tested the use of 89Zr-pan for PET in mice with implanted tumours. They injected the animals with 0.2 mCi of the tracer two weeks after tumour induction, and then delivered 5 Gy doses to the tumour on days 1 to 6 after administration, performing sequential PET/CT and radiotherapy. Assessing the tumour volume revealed that in control mice, which did not receive radiotherapy, tumour growth was considerable. The irradiated mice, on the other hand, showed clear tumour shrinkage following treatment.
The researchers also analysed the PET images to determine the stability of the PET signal in tumours following radiotherapy. They observed a progressive reduction in PET signal after irradiation compared with the signal from non-irradiated animals, with tumour uptake 50% lower in treated mice than controls. Fortunately, this decrease was not enough to affect the ability of BgRT to track the tumours.
To determine whether 89Zr-pan could track tumours in human patients, despite the observed signal decrease, the researchers applied two criteria for clinical BgRT: an activity concentration (AC) above 5 kBq/ml, and a normalized target signal (NTS) above 2.7.

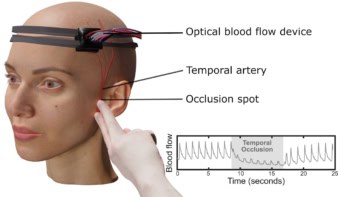
Biology-guided radiotherapy system spares critical organs
Natarajan pointed out that extrapolation from mouse to human could be more complex than simple scaling. However, based on a coarse rescaling of the mouse data to obtain hypothetical 89Zr-pan uptake values in equivalent human tumours, computations showed that the AC threshold was achieved on days 2 to 6 following tracer administration, while the NTS level was met on days 1 to 9. As such, the team concluded that BgRT could be feasible in equivalent human-sized tumours for roughly five consecutive days following a single tracer injection.
“The 89Zr immunoPET tracer has potential to guide BgRT,” Natarajan concluded. “What is important is that compared with FDG PET, long-lived-isotope-based BgRT has potential to use a single dose to track or treat for up to nine days, based on preclinical trial results.”