A machine learning model that combines data from two advanced imaging techniques can predict a patient’s risk of a future heart attack better than conventional clinical assessment. Writing in the Journal of Nuclear Medicine, the model’s developers report that contrast-enhanced CT angiography (CTA) and PET using the radiotracer 18F-sodium fluoride (18F-NaF) are complementary predictors of heart attack risk in patients with established coronary artery disease.
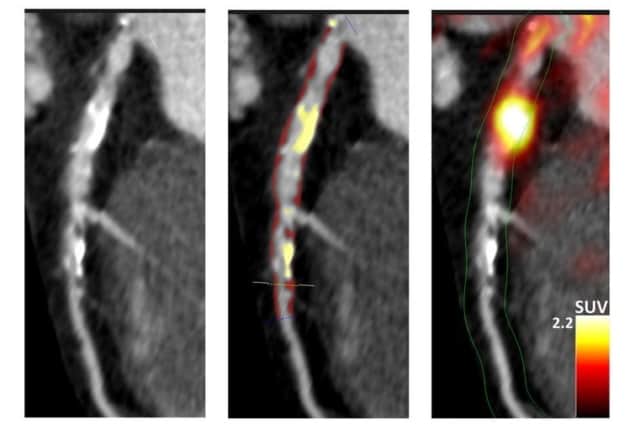
Predicting the future risk of heart attack is challenging, particularly in patients with coronary artery disease. Advanced imaging can help: CTA can be used to quantitatively analyse coronary plaque, while 18F-NaF PET can assess disease activity in the coronary arteries. Importantly, data from contrast-enhanced CTA and 18F-NaF PET can be acquired in a single imaging session on a hybrid PET/CT scanner.
A multinational, multidisciplinary team led by Piotr Slomka of the Cedars-Sinai Artificial Intelligence in Medicine division investigated whether the two methods produced complementary data that could provide superior predictive performance when combined. Their study examines 293 patients with established coronary artery disease receiving treatment at Cedars-Sinai and the University of Edinburgh’s Centre for Cardiovascular Science. The researchers followed the study group (84% male, aged 56 to 74 years) for a median 53 months. During this time, 23 patients had heart attacks, three of which were fatal.
Study participants initially underwent a comprehensive baseline clinical assessment, which included evaluation of their cardiovascular risk factor profile, followed by a coronary 18F-NaF PET and contrast CTA scan. Using a hybrid PET/CT scanner, the researchers acquired a non-contrast CT attenuation correction scan, followed by a 30-min PET scan, a low-dose non-contrast electrocardiogram (ECG)-gated CT and a contrast-enhanced ECG-gated coronary CTA.
The team used the PET data, with the aid of CTA-defined vessel boundaries, to calculate coronary microcalcification activity – a reproducible and robust measure of disease activity that’s predictive of disease progression and heart attack risk. They measured the coronary artery calcium score from the CT scans, and used the CTA scans for quantitative plaque analysis (calculating total, calcified, non-calcified and low-attenuation plaque volumes).
To analyse the data, the researchers developed three predictive machine learning models. The first, a clinical model, used baseline characteristics including age, sex, comorbidities, medication, biomarkers, past medical history and coronary calcium score. The second model was derived from the quantitative plaque analysis variables from CTA, while the third combined the clinical, CTA and 18F-NaF PET data.
The third model had the highest predictive value, followed by the second model. The clinical model showed limited predictive performance when incorporated into machine learning models.
“We showed that risk prediction does not depend on cardiovascular risk scores, stenosis severity or CT calcium scoring,” the researchers write. “Rather, the risk of myocardial infarction [heart attack] is primarily governed by the analysis of plaque type and plaque burden provided by coronary CTA and assessments of disease activity by 18F-NaF PET.”
Slomka says that combining 18F-NaF PET with anatomical imaging provided by CTA offers the potential to enable precision medicine by guiding the use of advanced therapeutic interventions. “Our study supports the use of artificial intelligence methods for integrating multimodality imaging and clinical data for robust prediction of heart attacks,” he explains.
“Our current efforts focus on patients who have experienced myocardial infarction or have stable multi-vessel disease,” he adds. “The risk stratification in patients with advanced coronary artery disease is particularly challenging. Therefore, in such patients, the uptake of 18F-NaF PET could provide important new information, and this novel imaging modality might address a critical clinical need.”
Routine eye scans could provide cost-effective screening for heart disease
Slomka is encouraged by other recent research investigating 18F-NaF uptake as a predictor of disease progression and adverse outcomes for patients with other cardiovascular conditions, including valvular heart disease and aortic aneurysms. He cites the PREFFIR study of 700 patients being followed for five years by the University of Edinburgh to evaluate the prognostic significance of 18F-NaF PET.
“This study shall soon determine whether, in patients hospitalized with myocardial infarction and angiographically proven multi-vessel coronary artery disease, 18F-NaF PET is a strong predictor of future recurrent heart attacks,” he explains.
The Slomka Research Lab is continuing research in this field, including analysis of another independent dataset and the development of further automation for analysis.