Brain tumours are notoriously difficult to treat, resisting conventional treatments such as radiation therapy, where the deliverable dose is limited by normal tissue tolerance. To better protect healthy tissues, researchers are turning to microbeam radiation therapy (MRT), which uses spatially fractionated beams to spare normal tissue while effectively killing cancer cells.
MRT is delivered using arrays of ultrahigh-dose rate synchrotron X-ray beams tens of microns wide (high-dose peaks) and spaced hundreds of microns apart (low-dose valleys). A research team from the Centre for Medical Radiation Physics at the University of Wollongong in Australia has now demonstrated that combining MRT with targeted radiosensitizers – such as nanoparticles or anti-cancer drugs – can further boost treatment efficacy, reporting their findings in Cancers.
“MRT is famous for its healthy tissue-sparing capabilities with good tumour control, whilst radiosensitizers are known for their ability to deliver targeted dose enhancement to cancer,” explains first author Michael Valceski. “Combining these modalities just made sense, with their synergy providing the potential for the best of both worlds.”
Enhancement effects
Valceski and colleagues combined MRT with thulium oxide nanoparticles, the chemotherapy drug methotrexate and the radiosensitizer iododeoxyuridine (IUdR). They examined the response of monolayers of rodent brain cancer cells to various therapy combinations. They also compared conventional broadbeam orthovoltage X-ray irradiation with synchrotron broadbeam X-rays and synchrotron MRT.
Synchrotron irradiations were performed on the Imaging and Medical Beamline at the ANSTO Australian Synchrotron, using ultrahigh dose rates of 74.1 Gy/s for broadbeam irradiation and 50.3 Gy/s for MRT. The peak-to-valley dose ratio (PVDR, used to characterize an MRT field) of this set-up was measured as 8.9.
Using a clonogenic assay to measure cell survival, the team observed that synchrotron-based irradiation enhanced cell killing compared with conventional irradiation at the same 5 Gy dose (for MRT this is the valley dose, the peaks experience 8.9 times higher dose), demonstrating the increased cell-killing effect of these ultrahigh-dose rate X-rays.
Adding radiosensitizers further increased the impact of synchrotron broadbeam irradiation, with DNA-localized IUdR killing more cells than cytoplasm-localized nanoparticles. Methotrexate, meanwhile, halved cell survival compared with conventional irradiation.
The team observed that at 5 Gy, MRT showed equivalent cell killing to synchrotron broadbeam irradiation. Valceski explains that this demonstrates MRT’s tissue-sparing potential, by showing how MRT can maintain treatment efficacy while simultaneously protecting healthy cells.
MRT also showed enhanced cell killing when combined with radiosensitizers, with the greatest effect seen for IUdR and IUdR plus methotrexate. This local dose enhancement, attributed to the DNA localization of IUdR, could further improve the tissue-sparing capabilities of MRT by enabling a lower per-fraction dose to reduce patient exposure whilst maintaining tumour control.
Imaging valleys and peaks
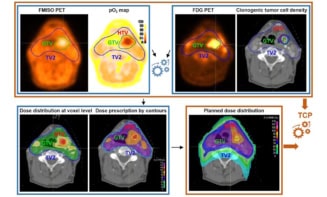
To link the biological effects with the physical collimation of MRT, the researchers performed confocal microscopy (at the Fluorescence Analysis Facility in Molecular Horizons, University of Wollongong) to investigate DNA damage following treatment at 0.5 and 5 Gy. Twenty minutes after irradiation, they imaged fixed cells to visualize double-strand DNA breaks (DSBs), as shown by γH2AX foci (representing a nuclear DSB site).

The images verified that the cells’ biological responses corresponded with the MRT beam patterns, with the 400 µm microbeam spacing clearly seen in all treated cells, both with and without radiosensitizers.
In the 0.5 Gy images, the microbeam tracks were consistent in width, while the 5 Gy MRT tracks were wider as DNA damage spread from peaks into the valleys. This radiation roll-off was also seen with IUdR and IUdR plus methotrexate, with numerous bright foci visible in the valleys, demonstrating dose enhancement and improved cancer-killing with these radiosensitizers.
The researchers also analysed the MRT beam profiles using the γH2AX foci intensity across the images. Cells treated with radiosensitizers had broadened peaks, with the largest effect seen with the nanoparticles. As nanoparticles can be designed to target tumours, this broadening (roughly 30%) can be used to increase the radiation dose to cancer cells in nearby valleys.
“Peak broadening adds a novel benefit to radiosensitizer-enhanced MRT. The widening of the peaks in the presence of nanoparticles could potentially ‘engulf’ the entire cancer, and only the cancer, whilst normal tissues without nanoparticles retain the protection of MRT tissue sparing,” Valceski explains. “This opens up the potential for MRT radiosurgery, something our research team has previously investigated.”
First patients treated using minibeam radiation therapy
Finally, the researchers used γH2AX foci data for each peak and valley to determine a biological PVDR. The biological PDVR values matched the physical PVDR of 8.9, confirming for the first time a direct relationship between physical dose delivered and DSBs induced in the cancer cells. They note that adding radiosensitizers generally lowered the biological PVDRs from the physical value, likely due to additional DSBs induced in the valleys.
The next step will be to perform preclinical studies of MRT. “Trials to assess the efficacy of this multimodal therapy in treating aggressive cancers in vivo are key, especially given the theragnostic potential of nanoparticles for image-guided treatment and precision planning, as well as cancer-specific dose enhancement,” senior author Moeava Tehei tells Physics World. “Considering the radiosurgical potential of stereotactic, radiosensitizer-enhanced MRT fractions, we can foresee a revolutionary multimodal technique with curative potential in the near future.”