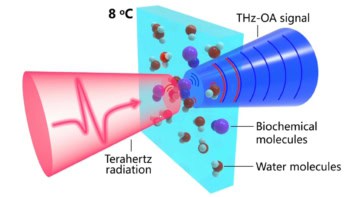
An inter-disciplinary research team headed up at the University of California, Los Angeles (UCLA) has pioneered a new, minimally invasive approach to skin cancer treatment. The technique uses a novel microneedle patch to facilitate the delivery of cold plasma to tumours – and could make immunotherapy more effective for treating melanoma (PNAS 10.1073/pnas.1917891117).
Prolonged survival
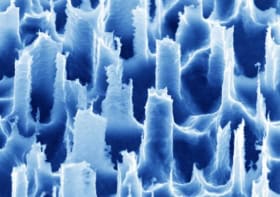
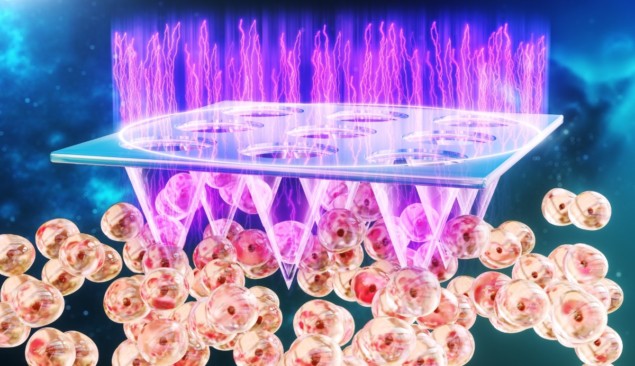
As part of the work, the researchers engineered a thumb-sized patch containing more than 200 hollow-structured microneedles. They used the patch to deliver cold atmospheric plasma, a unique type of ionized gas that can kill cancer cells, to tumour tissues in mice with melanoma. The microneedles also deliver immunotherapeutics – immune checkpoint inhibitors – directly to the tumour.
Treatment with the patch significantly delayed tumour growth in the mice and prolonged survival. In addition to inhibiting growth of the targeted tumour, the researchers found that the technique was also capable of reducing the growth of tumours that had already spread to other parts of the body.
As senior author Zhen Gu explains, through this thumb-sized device, cold plasma can efficiently trigger cancer cell death, which initiates a tumour-specific immune response. This immune response is further augmented by the immunotherapeutics released from the device.
“We found that this local device can inhibit the growth of the tumour and prolong the survival of the mice,” says Gu. “More importantly, it could also trigger the systemic immune response to inhibit the growth of distant tumours. The study is also the first to demonstrate that cold plasma can be used in synergizing cancer immunotherapy.”
Clinical potential
Although Gu believes that immunotherapy shows great promise in treating cancers, he stresses that several challenges still remain – for example, the fact that immune checkpoint blockade therapy “overall has low objective response rates and is also associated with systemic toxicities”. In response to these ongoing limitations, he reveals that he and the rest of the research team were motivated by a desire to engineer approaches capable of boosting the overall efficacy of cancer immunotherapy.
“The local device we reported could enhance the anti-tumour efficacy and potentially minimize the side effects related to immune checkpoint blockade therapy,” Gu says.

A versatile technology
Moving forward, Gu is confident that the new strategy holds potential for clinical treatment of cancer. However, on a more cautious note, he stresses that although the research team obtained several promising results in preclinical models, the new technique will have to go through further testing and approvals before it could be used in humans.
“Factors to be considered in the future study are the control of the cold plasma – such as time, intensity and frequency – and optimization of the microneedle device, as well as the dosage of cancer immunotherapeutics,” he says.
And this strategy could potentially be extended beyond melanoma treatments. “Integrated with other treatments, this minimally invasive method could be extended to treat different cancer types and a variety of diseases,” Gu adds.