Researchers in Israel have developed and tested a fibre-optic evanescent wave spectroscopy (FEWS) system that can non-invasively identify and characterize skin cancers. They successfully identified cancerous lesions on patients’ skin by touching the suspicious regions for 30 s with an optical fibre connected to a mid-infrared (IR) spectrometer.
An estimated 300,000 cases of melanoma and more than one million cases of non-melanoma skin cancer were diagnosed in 2018, according to the World Cancer Research Fund and the American Institute for Cancer Research. Suspicious lesions are usually identified by dermatologists using a dermascope, a handheld optical magnifier, and are subsequently diagnosed based on pathological analysis of biopsied tissue. This process, however, is invasive, costly, time-consuming and dependent upon the skill of the physician.
To address these shortfalls, Abraham Katzir of Tel Aviv University and co-researchers are working to create an accurate, affordable clinical system that can identify skin cancers in near-real-time and could be used by dermatologists for reliable screening of suspicious lesions. Writing in Medical Physics, the researchers describe their achievements to date.
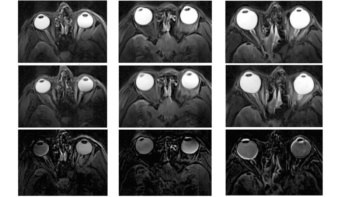
The FEWS system is based on a mid-IR spectrometer and a long, U-shaped, mid-IR transmitting AgCIBr fibre. The fibre, developed by Tel Aviv University’s applied physics group, is flexible, non-toxic, non-hygroscopic and highly transparent in the mid-IR. The system operates in the 3–30 μm spectral range, to measure the mid-IR absorption spectra of tissues. To record an absorption spectrum, the centre of the U-shaped fibre is simply brought into contact with the skin.
Patient studies
The researchers aimed to use the FEWS system to detect and identify three skin cancers: melanoma, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). For 90 patients in the dermatology department of the Tel Aviv Sourasky Medical Center, they measured the absorption spectra of each suspicious skin lesion and the surrounding healthy tissue, a process that took about 30 s per measurement.
The absorption spectra of the measured samples exhibited several peaks in the mid-IR region. Unique peaks at similar wavenumbers and within specific spectral ranges, were easily identified by the naked eye as signatures of melanoma, BCC or SCC. The team created “biochemical fingerprints” for samples of melanoma, BCC, SCC and healthy tissue, based on differences in the absorption spectra. These spectra corresponded with the pathology of the patients’ tissue biopsies, which included five melanomas, seven BCCs and three SCCs.
In a recent refinement of their diagnostic method, the researchers developed an algorithm to analyse the spectra and deliver the results. For melanoma, this algorithm achieved 100% sensitivity, specificity and accuracy.
One potential obstacle with this approach is that mid-IR radiation only penetrates only a few microns into the stratum corneum, the upper layer of the skin. The researchers suggest that this thin layer would include cells that have migrated upwards from deeper malignant lesions.
“This study confirmed that the melanoma-affected cells migrate from the layers of the skin to the thin top layer,” explains Katzir. “We were able to use mid-IR spectroscopy on this very thin layer of skin to detect these cells, without breaking the skin, and from that to determine the type of cancer present. The differences among the cancer types were large and were immediately noticed by simple comparison of the spectra. This non-invasive ‘spectroscopic pathology’ may, in the future, replace the standard invasive biopsy.”

Katzir tells Physics World that the team is planning to conduct a larger number of experiments in a collaboration with the Sheba Medical Center, which has a large medical clinic dedicated to skin cancer.
“Our main interest is to develop a system that will automatically diagnose lesions, independent of the skill of the physician,” Katzir explains. “It will determine if the lesions are cancerous, and conclude whether they are melanoma or less lethal cancers, all in real-time and in the clinic. The dermatologist community and the medical authorities are looking for a method that will diagnose, with a success rate of more than 95%, both malignant and benign skin lesions. If we succeed, we will try to get an approval for the method and then we will be ready for commercialization.”
The next step will be to collect more data to improve the data analysis. The system also needs to be refined. The researchers plan to replace the commercial mid-IR spectrometer with a quantum cascade laser (QCL)-based system that will only cover the spectral range of interest, have higher intensity and be more compact. They also plan to improve their software algorithms to better detect melanoma and other pathologies, and to generate these findings automatically.
“We hope to develop a system that is small, lightweight, rugged, very easy to operate and, most importantly, inexpensive,” says Katzir. “We want to reduce the cost to be less than £4000 (or $5000), so that small clinics can afford to purchase it. This system has the potential to make a sea change in the diagnosis of skin cancers and possibly other types of cancer. This is our goal.”