A technology called monochromatic X-ray imaging could reduce radiation dose per mammogram by a factor of five to 10 times, according to a research review published in the European Journal of Radiology.
Michael Fishman from Boston University and Madan Rehani from Massachusetts General Hospital proposed that contrast-enhanced digital mammography with monochromatic X-rays provides a simpler and more effective imaging technique at substantially lower radiation dose.
“Lowering radiation dose by a factor of five to 10 while maintaining image quality implies a major reduction in total exposure from breast cancer screening and dramatically less risk of radiation-induced cancers in at-risk women,” Fishman and Rehani write.
X-ray systems of today are largely based on the hot cathode X-ray tube first developed by William Coolidge in 1913, and this technology remains the universally accepted method for breast cancer detection due to its wide availability, low cost and repeatability, the authors write.
However, the radiation delivered by the technique has been a focus of debates regarding possible cancer risk associated with breast screening. Monochromatic X-ray imaging is a recent development that could reduce cancer risk in mammography by dramatically reducing radiation dose.
While conventional radiography systems use multiwavelength X-ray emission extending over a broad energy band, monochromatic X-rays use two X-ray emission processes to generate monochromatic X-ray beams. The first beam is similar to conventional X-ray, as high-energy electrons bombard a metal target to emit broadband X-ray energies.
The second emission process involves the concentration of X-rays onto a small, thin-foil metallic target. This target emits monochromatic X-rays via fluorescence, and its elemental composition can be identified by its energy.
“It is especially important for examining dense breast tissue where image quality frequently is suboptimal and limited in sensitivity,” the authors write.
Fishman and Rehani wanted to examine details from previous studies about monochromatic X-ray technology and its application to breast imaging. They analysed study results using a prototype system developed by Eric Silver from Imagine Scientific for breast imaging that generates such X-rays through fluorescence emission.
“[We] anticipate its [system’s] first use in the clinic within several months,” Silver tells AuntMinnie.com.
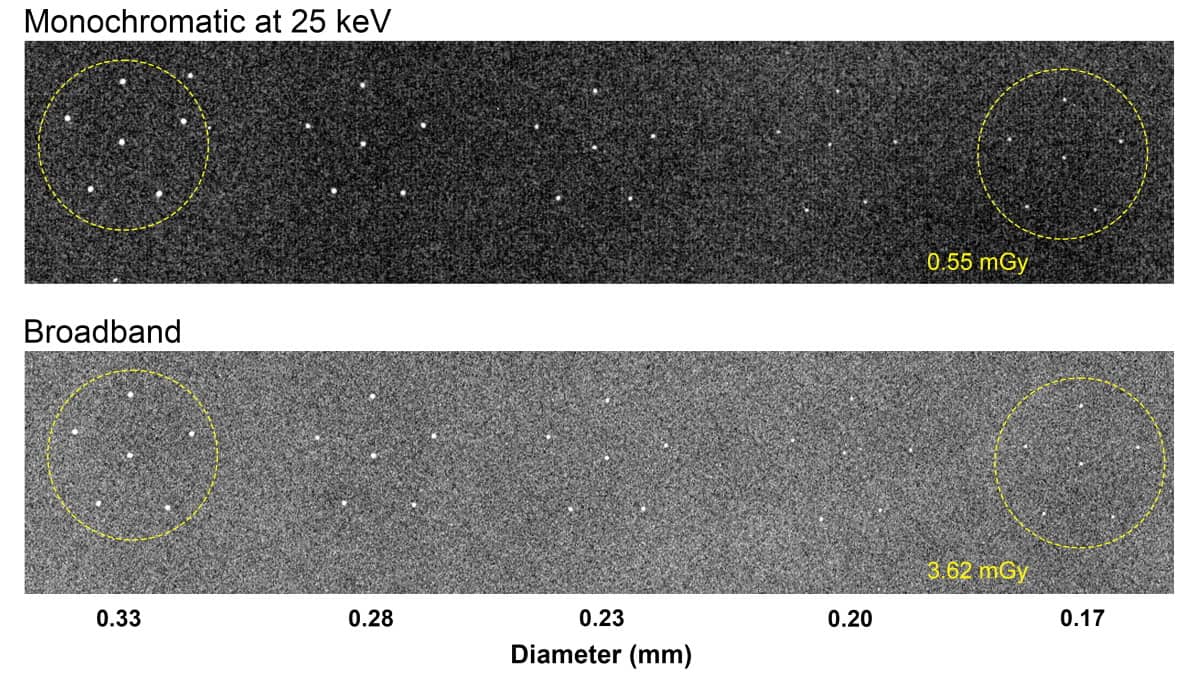
Fishman and Rehani also assessed signal-to-noise ratio as a measure of image quality at different doses in breast phantoms of different sizes, and reviewed the comparison of parameters with a standard mammography system.
Along with finding a five- to 10-times reduction in radiation dose, the researchers found promise for a phantom simulating thick breasts (9 cm). For such simulations, the signal-to-noise ratio for monochromatic X-rays was 2.6 times higher and the radiation dose was 4.2 times lower than conventional X-rays.
“For the conventional broadband system to equal the signal-to-noise ratio of the monochromatic system, it would require a dose of 19 mGy, 29 times higher than the dose delivered by the monochromatic system,” they note.
Monochromatic X-ray source could make mammograms safer
Rehani tells AuntMinnieEurope.com that the technology is ready for human imaging and has the potential to replace millions of X-ray tubes in the world currently in breast imaging, CT, fluoroscopy and radiography machines. He also says that more funding and clearances are needed before it can be widely accepted.
“There is a plan to upgrade technology to reduce exposure time which is again more of a financial issue rather than development of technology,” he says.
Silver tells AuntMinnieEurope.com that the prototype system is being adapted for use at higher energies to address CT applications with and without contrast.
- This article was originally published on AuntMinnieEurope.com ©2021 by AuntMinnieEurope.com. Any copying, republication or redistribution of AuntMinnieEurope.com content is expressly prohibited without the prior written consent of AuntMinnieEurope.com.