Space travel causes long-lasting changes in the brain’s white matter volume and the shape of the pituitary gland, US researchers report after a longitudinal study of 11 astronauts. The findings may have health implications for the crew of future, long-haul space missions – and may help shine light on related conditions back on Earth.
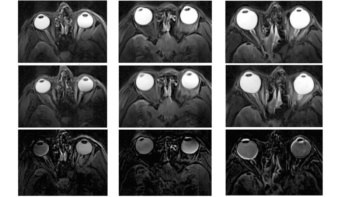
Following expeditions to the International Space Station, more than half of astronauts reported experiencing changes to their vision – most commonly in the development of farsightedness, but also manifesting as mild headaches and, in severe cases, as a loss in both near and distant acuity. Examination of patients with this “spaceflight associated neuro-ocular syndrome” has revealed a number of structural changes, including swelling of the optic nerve and retinal haemorrhage.
“When you’re in microgravity, fluid such as your venous blood no longer pools toward your lower extremities, but redistributes headward,” explains Larry Kramer, a radiologist from the University of Texas. “That movement of fluid toward your head may be one of the mechanisms causing changes we are observing in the eye and intracranial compartment.”
In their study, Kramer and colleagues conducted a series of brain MRI scans on 11 astronauts – 10 men and one woman – prior to and after missions to the International Space Station. The team found that significant time spent in the orbiting laboratory’s microgravity environment caused the crew’s brain and cerebrospinal fluid volumes to expand – an effect that was found to persist at least a year later.
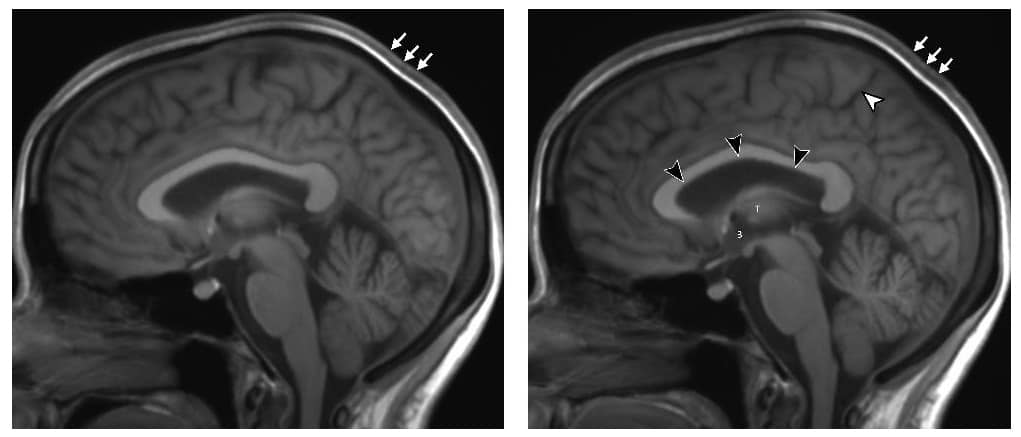
“What we’ve identified that no one has really identified before is that that there is a significant increase of volume in the brain’s white matter from pre-flight to post-flight,” Kramer says. “White matter expansion is in fact responsible for the largest increase in combined brain and cerebrospinal fluid volumes post-flight.”
The researchers also observed changes in the shape of the pituitary gland in many of the test subjects following their spaceflights – with the gland becoming smaller and flatter.
A further change was identified in the rate at which cerebrospinal fluid flows through a narrow channel in the brain called the cerebral aqueduct, which connects the brain’s four ventricles. A similar phenomenon is seen in a condition called normal pressure hydrocephalus – in which fluid builds up in the ventricles – which causes symptoms including dementia, difficulties walking and bladder control problems. The astronauts, however, are not exhibiting these symptoms – although the team suspect that both conditions may share a similar mechanism of injury.
Regardless, according to Kramer, it is not clear whether the astronauts’ intracranial changes might be reversible. “The best solution is probably prevention,” he concludes.
“Currently we do not understand the clinical significance, if any, of these changes in brain structure, which highlights the need for further research,” comments Donna Roberts, a radiologist from the Medical University of South Carolina, who was not involved in the present study. “Determining the cause of the spaceflight-associated neuro-ocular syndrome will be important in ensuring the health of our astronauts on the International Space Station and for planning longer-duration missions, such as a crewed mission to Mars.”
“Spaceflight-associated neuro-ocular syndrome remains among NASA’s top health risks for long-duration spaceflight,” agrees physiologist Damian Bailey of the University of South Wales. The study “lends additional support to the evolving albeit controversial hypothesis that [its] symptoms are related to chronic intracranial hypertension,” he adds, noting that the findings are not only relevant for astronauts, but may also help inform the clinical management of hospital patients suffering from related symptoms.”
MRI reveals how space travel alters the brain
With their initial study complete, the researchers are now moving to investigate potential countermeasures that might be used to prevent intracranial changes during spaceflight – such as creating artificial gravity using a large centrifuge, or applying negative pressure to the lower extremities to counteract the headward shift of fluids under microgravity.
“We will be using head-down tilt bedrest studies as an analogue of fluid shift seen in microgravity,” Kramer says, explaining that these conditions can reproduce the same intracranial and orbital changes. “If countermeasures work in the analogue studies they may potentially work in microgravity.”
The research is described in the journal Radiology.