Researchers from the University of Torino have designed a protein that can repair abnormal tumour blood vessels, and by doing so, improve the tumour’s treatment with chemotherapy. Treating cancerous tumours with drugs can be difficult as the blood vessels surrounding them become altered. This results in improper blood flow, or vascularization, to the tumour. This in turn means that chemotherapies delivered via the circulatory system are less effective. As such, investigators are trialling treatments to normalize tumour vasculature and improve chemotherapy efficacy.
SEMA3A proteins (which regulate blood vessel formation) can normalize blood vessels by acting through their primary receptors, neuropilin-1 (NRP-1) and plexin (PLXN) receptors. Unfortunately, some independent studies have shown that SEMA3A may also have serious adverse effects, due to its action on the NRP-1 receptor.
Rational design of a “superagonist”
Now, a research collaboration led by Guido Serini, Enrico Giraudo and Luca Tamagnone has used rational design to alter the SEMA3A protein. This stops it binding to NRP-1, while maintaining its positive blood vessel response through the PLXNA4 receptor (Sci. Transl. Med. 10.1126/scitranslmed.aah4807).
SEMA proteins are well characterized, including the specific domains that bind to NRP-1 and PLXN receptors. The researchers first showed that removal of the NRP-1 binding domain from SEMA3A did not alter its anti-tumour effect. This suggested that the blood vessel normalization was not entirely dependent on NRP-1 signalling. Instead, the effects came from other SEMA3A-receptor interactions, such as those with PLXNA4.
As the interaction between SEMA3A and PLXNA4 is relatively weak, the researchers sought a way to increase the binding affinity. By analysing high-resolution crystallography data of closely related proteins, they could look at the interface between SEMA3A and PLXNA4 and their amino acids.
They found that substituting the alanine at position 106 with a charged lysine created a mutant protein with higher binding affinity to PLXNA4. The mutated protein, SEMA3A_A106K, also inhibited migration of endothelial cells, the main component of blood vessels.
Boosting chemotherapy
The researchers then used a purified version of the mutant protein to assess its clinical efficacy in treating a mouse model of pancreatic cancer. The treatment significantly decreased tumour growth, as well as improving survival rates compared with control mice. Importantly, the therapy did not cause any detectable signs of the toxicity that had been present in the initial NRP-1-binding SEMA3A protein.
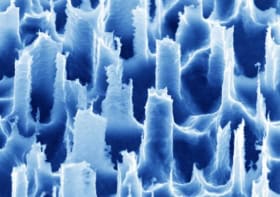
To determine if these beneficial effects were due to blood vessel normalization, the researchers assessed the effects of SEMA3A_A106K on blood vasculature in two mouse models of pancreatic cancer. They observed significant vascular normalization, which promoted tumour perfusion and reduced tumour hypoxia.
Subsequently, they gave the mice SEMA3A_A106K in conjunction with the common chemotherapeutic gemcitabine. This co-administration inhibited tumour growth and reduced metastases more than each individual agent. They also noted that SEMA3A_A106K alone displayed stronger anti-metastatic activity than chemotherapy alone. From this, they concluded that the protein was indeed vessel-normalizing and improved the delivery of chemotherapeutic drugs in these models of pancreatic cancer.
This research has shown the successful rational design and mutation of the endogenous protein SEMA3A. The “superagonist” SEMA3A mutant normalized tumour vasculature selectively through PLXNA4, which in turn improved the effects of the drug gemcitabine. With increased evidence that normalizing tumour vasculature can improve patient outcome, this research is a step towards improved therapies for difficult-to-treat cancers.