
At a recent innovation webinar hosted by the UK’s National Physical Laboratory (NPL), speakers shared details of some of the breakthrough technologies being developed and commercialized by UK companies and laboratories. Two of the presentations described novel medical imaging developments that could improve cancer diagnosis and treatment, and examined how the resulting devices could get into the hands of users and make a difference to society.
Surgical guidance system
Lightpoint Medical, a specialist in precision-guided robotic cancer surgery, is developing miniaturized sensing tools for intra-operative cancer detection. Kunal Vyas, Lightpoint’s head of research, shared the rationale behind the company’s SENSEI cancer surgery guidance system.
“What is shocking, is that when you go for surgery, the surgeon will only use their sight and touch to remove your cancer,” Vyas explained. “The lack of interoperative tools to detect cancer means that tumour tissue is frequently missed, or in other cases, healthy tissue is needlessly removed.” He noted that in prostate cancer surgery, for example, one in four patients has some tumour left behind and one in six experience complications.
To address this, Lightpoint Medical is developing tools to help surgeons more accurately detect and remove cancer during surgery. The company’s SENSEI system combines miniaturized sensors with cancer-targeting radiotracers developed and approved for use in PET and SPECT scans, incorporated into a single-use 12 mm-diameter probe.
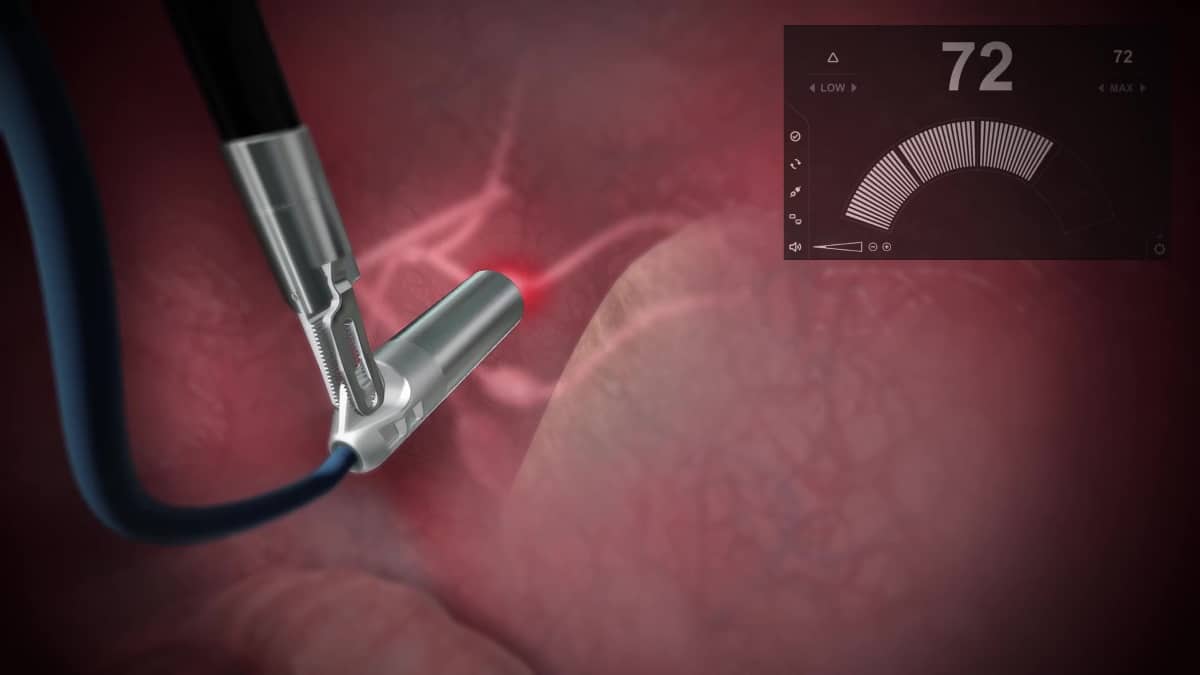
Prior to surgery, the patient is injected with the radiotracer, which accumulates in cancerous tissue. The probe then detects emissions from these radiotracers to help surgeons locate cancer in real time in the operating room. “This allows cancer surgery to be molecularly targeted using state-of-the-art diagnostic tracers,” says Vyas.
The SENSEI system can be used during all types of cancer surgery, including keyhole and robotic surgery, and is suited for numerous cancer types including prostate, lung, colorectal and gynaecological cancers. Assessments of the system’s performance in a preclinical setting demonstrated 100% identification rate at 2.5 cm tissue depth. The next step will be to move into clinical trials, with the first trials aimed at improving outcomes for patients with prostate cancer.
“I think precision guidance is the next revolution in surgery,” said Vyas. He noted, however, that uptake of new surgical technologies can be quite slow, particularly when it is a device that’s actually inserted into the body. “Surgeons and medical professionals are rightfully quite conservative, there’s quite a high-risk profile in introducing something new into the operating room.”
Lightpoint is expecting to receive US and EU market clearance later in 2020, said Vyas, adding that the company has secured £3m in its latest funding round. “We’ve been really grateful for having a combination of private equity and public funds to make this happen,” he said.
Ultrasound breast imaging
NPL Fellow Bajram Zeqiri discussed another medical imaging technology: ultrasound computed tomography (UCT), which could improve outcomes for breast cancer patients. “In the UK’s national breast cancer screening programme, three million women are invited annually for compression X-ray mammography,” he said. “Of these, only around 75% accept, partly due to the discomfort of the procedure.” But, as with all cancers, early detection is essential – increasing survival rates, as well as lowering treatment costs and reducing potential treatment-related side-effects.
And X-ray mammography has other shortcomings. It generates false positives, with 20,000 unnecessary biopsies performed each year, and is not ideal for imaging dense breast tissue, due to a significant cloaking effect on images. When such “white out” occurs on mammograms, ultrasound is used as an adjunct, as it is better at differentiating between dense background breast tissue and cancers.
So why is ultrasound not used as a primary screening tool? Likely because conventional ultrasound only targets small regions of tissue, requires high operator skills, and the detectors used in current systems also give a high level of false positives, explained Zeqiri. Some of these obstacles could be overcome by using UCT, which works by transmitting ultrasonic sound waves through the breast and exploits the higher acoustic attenuation and speed-of-sound of malignant tissue as its contrast mechanism.
Various UCT systems are currently under development, but their reliance on conventional piezoelectric technology means that images are still subject to artefacts. So NPL has developed a completely new type of UCT detector that uses the pyroelectric effect to measure ultrasonic power accurately. “The new detector will support near error-free quantitative acoustic attenuation tomography,” said Zeqiri.

Using a laboratory platform, Zeqiri and colleagues demonstrated that UCT with the pyroelectric detectors could create quantitative images of breast phantoms, with excellent correlation to ground-truth values and X-ray images. They have also recorded the first in vivo measurements (not images) from volunteers, to generate engineering data for future development of the technology.
Ultimately, the UCT device will enable full 3D quantitative breast scanning in just 5–10 minutes. The system, which will be suitable for measuring dense breast tissue, will also employ AI to compare the scans with a reference library of images linked to known pathologies – leading to improved automated diagnosis and far fewer false positives.
Achieving this, explained Zeqiri, requires three phases of work: recording the first images from volunteers; building a mark II system for comparison with conventional imaging on cancer patients; and then performing a large multicentre trial. He also highlighted the need for investment, noting that the biggest obstacle at the moment is funding for the second phase. “The problem is funders want to see proof, but you need funding to actually demonstrate that it works.”
Zeqiri expects that the new UCT system will first be used diagnostically to identify specific cancer types and reduce biopsies, before ultimately being employed for screening. “It could be very versatile because it uses non-ionizing radiation so it’s safe. It could be deployed anywhere, in a GP’s surgery or even in a fitness centre. It’s got real potential,” he concluded.
The session also included presentations by speakers from three other organizations.
- Graham Farnsworth from the Defence Science and Technology Laboratory (Dstl) described a forensic technology that can recover fingerprints in scenarios where no other technique can do so. He explained how a collaborative approach helped transition the technology from a development at Loughborough University into a commercial product being sold to multiple users, and even applied by law enforcement agencies to reopen cold cases.
- Vivienne Parry, head of engagement at Genomics England introduced the 100,000 genomes project, which has now sequenced around 120,000 genomes from 70,000 patients with either a rare disease or cancer. The project, which collected 21 petabytes of clinical data, enabled a 25% increase in the diagnostic rate for rare diseases and, for cancers, was able to find an actionable variant in nearly two-thirds of patients. The legacy of this project is the National Genomic Research Library, a constantly refreshed dataset of genomes and associated clinical data for academic and commercial research.
- Claire A Fowler, process development scientist at Leaf Expression Systems, discussed the use of plant-based expression to produce proteins, antibodies, enzymes, vaccines and complex natural products for research and commercial applications. The company focuses on using their plant-produced expression technology to accelerate research and lower costs for developing and manufacturing therapeutic drugs, vaccines and diagnostics for human and animal health.
The next NPL innovation webinar takes place on 8 October and will focus on AI and robotics, fusion power and nuclear.



