A team of US-based researchers has demonstrated how low-cost, non-invasive diffuse correlation spectroscopy (DCS) can improve the assessment of cerebral blood flow in children with sickle cell disease – a genetic blood disorder that can have a substantial impact upon the brain.
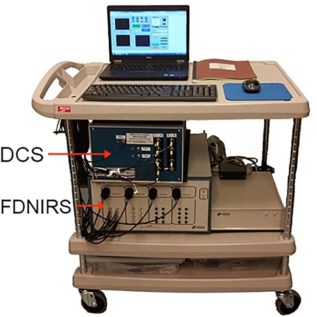
DCS is an optical technique that employs near-infrared light to relate intensity fluctuations of multiply scattered reflected light detected at the tissue surface to a blood flow index (BFI) in the underlying tissue. The researchers, based at the Georgia Institute of Technology, Emory University and Children’s Healthcare of Atlanta, used DCS to quantify brain blood flow in 11 children with sickle cell disease along with 11 healthy controls. As expected, they found that BFI was significantly higher in subjects with sickle cell disease than in the control group (Neurophotonics 10.1117/1.NPh.6.3.035006).
“Previous studies using other neuroimaging modalities have shown that kids with sickle cell disease have elevated blood flow in their brain as a compensatory mechanism to improve oxygen delivery in the face of chronic anaemia,” says co-author Erin Buckley from Georgia Tech and Emory University School of Medicine. “We found that DCS was sensitive to expected elevations in brain blood flow with sickle cell disease.”
In Buckley’s view, DCS offers numerous other advantages over traditional neuroimaging modalities that measure brain blood flow. To begin with, she highlights the fact that the manufacturing cost of a DCS system – in the region of $40,000 for the system used in the study – is orders of magnitude lower than modalities such as MRI or PET. She also observes that DCS does not involve exposure to contrast agents or ionizing radiation, and is “well tolerated in children of all ages without the need for sedation”.
Low-cost tool
Moving forward, first author Paul (Seung Yup) Lee, a postdoctoral fellow in Buckley’s group, points out that DCS may provide a simple, low-cost tool for bedside assessment of brain blood flow. In particular, he and the research team envisage promising clinical potential for DCS in children with sickle cell disease.
“Sickle cell disease can have profound effects on the brain, including a significantly elevated risk of stroke,” Lee explains. “DCS measurements could be routinely completed at a baseline when in good health, tracked over time, and monitored when ill to mitigate risk of stroke by identifying warning signs of abnormal brain blood flow compromise and enabling timely therapeutic intervention. In short, we envision that DCS could one day be for paediatric sickle cell disease what the blood glucose monitor is for diabetes.”
On a more cautious note, Lee stresses that, at present, DCS is strictly a research tool – and that, although a handful of companies have begun to commercialize the technology, such systems are not yet FDA approved, meaning they remain targeted at research use. Even so, he argues that if the research team continues to identify key applications that can potentially improve patient care, they are “confident the technology will eventually be implemented in routine clinical practice”.
From a technology development standpoint, Lee also reveals that the team want to better understand the potential effects of haematocrit (the ratio of the volume of red blood cells to the total volume of blood) on DCS measurements, a topic he believes is particularly relevant in sickle cell disease, given the wide range of haematocrit levels seen clinically in these patients.
“We are currently working on benchtop experiments in tissue-simulating phantoms and validation studies against MRI in order to better understand these effects,” he says.
Buckley reveals that another technology development aim for the future is to “continue to push the envelope” in terms of lowering the costs of manufacturing a DCS system and making the system wearable and wireless.
“From a clinical research standpoint, our next steps are to demonstrate that these non-invasive measurements of brain blood flow we are making may actually be helpful in clinical decision making,” she adds. “We have several prospective clinical studies in the works to explore the utility of these measurements.”