Robotic platforms enable surgeons to perform complex – usually minimally invasive – procedures with more precision, flexibility and control than possible using conventional techniques. To maximize its effectiveness, minimally invasive surgery requires not only well-engineered robotic instruments, but also precise target definition, achieved via image-guidance technologies.
Prior to surgery in complex anatomical regions, nuclear medicine techniques such as SPECT/CT or PET/CT can be used to create a map of the patient showing the number and location of surgical targets, such as tumours or tumour-related lymph nodes. Such maps are generated by detecting injected radiotracer that localizes in tumour cells.
The same radiotracer also enables “radio-guidance” during robot-assisted, minimally-invasive surgery. To detect the radioactive signal within the patient during the surgery itself, surgeons can use a new device known as a DROP-IN gamma probe, which was developed specifically for minimally invasive robotic procedures. The DROP-IN is a small tethered probe that detects gamma rays and generates a sound (and numeric readout) when it is close to a lesion containing radiotracer. The probe is positioned by the surgeon via the robot and is far more flexible than traditional laparoscopic gamma probes, allowing better localization of target lesions.
“The DROP-IN gamma probe is something we’ve been working on since 2014,” says Matthias van Oosterom from the Interventional Molecular Imaging laboratory at Leiden University Medical Center. “Since roughly 2018, we have been performing proof-of-concept studies in patients using this probe and have evaluated it in over 40 patients so far.”
Despite the availability of a patient map and intraoperative confirmation with the DROP-IN probe, it can still remain challenging to find an efficient route through the patient during surgery, especially when the surgical targets are seated at deep and complex locations. “In analogy to GPS navigation integrated in most modern cars, navigation is expected to take surgical localization to the next level,” says van Oosterom.
The challenge with surgical navigation, however, is that locating the exact position of the surgical instruments within the map of the patient (the SPECT/CT scan) is difficult, as many tool-tracking technologies aren’t suitable for use in a laparoscopic setting. To address this, van Oosterom and colleagues investigated the use of real-time fluorescence-based optical navigation of a DROP-IN gamma probe during robotic surgery. They tested the approach in phantoms and in pigs, reporting their results in the Journal of Nuclear Medicine.
Fluorescence tracking
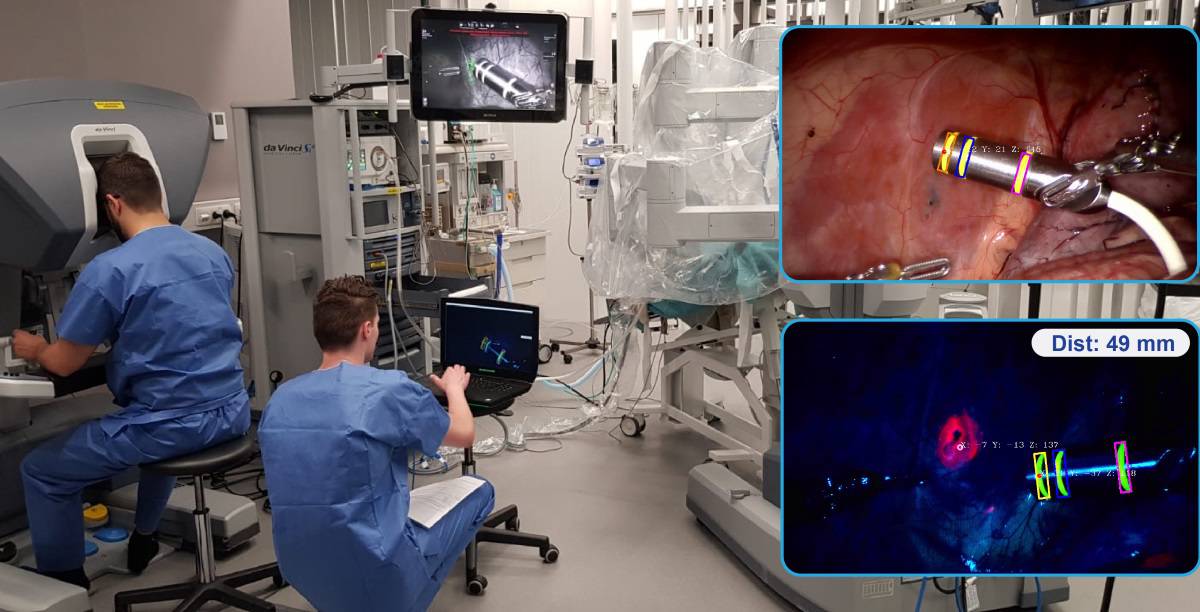
To ease clinical translation, the team combined the DROP-IN gamma probe with two clinically approved technologies: a Da Vinci robot equipped with a Firefly Si fluorescence laparoscope; and a declipseSPECT navigation system.
To track the DROP-IN gamma probe, the researchers marked its housing with a three-ring pattern of fluorescein, which fluoresces in yellow. Automated detection of this fluorescence allowed the pose of the DROP-IN tip to be estimated with respect to the Firefly laparoscope. The declipseSPECT was then used to determine the pose of the Firefly and the patient within the operating room, based on reference targets attached to the Firefly and the patient.
The researchers first tested their navigation concept using a torso phantom containing bones, artery structures and pelvic lymph nodes filled with radioactive tracer. They fixed the navigation reference target on the phantom’s hip and acquired three SPECT/CT scans, using the reference target to register the scans within the operating room.
The view inside the phantom, as seen on the robotic surgical console, included an augmented reality overlay of the lesions segmented from the SPECT/CT scan. Maintaining a direct line-of-sight between the Firefly and the DROP-IN enabled real-time calculation of the distance between the targeted lesion and the DROP-IN tip, with audible feedback confirming effective navigation.
To investigate DROP-IN tracking in a real-life surgical setting, the researchers next performed robot-assisted laparoscopic surgery on pigs, in the surgical training facility of Orsi Academy. By depositing indocyanine green (ICG, which fluoresces in pink) in the abdominal wall they created surgical targets to which the DROP-IN probe was navigated.
In fluorescence-imaging mode, both the fluorescein markers on the DROP-IN probe and the ICG deposits were visible. Uniquely, fluorescein and ICG fluorescence could be excited simultaneously and the emissions distinguished using the raw signal output of the Firefly camera, allowing the surgeon to visually confirm the localized lesions during navigation. There was no obvious difference in intensity between the two fluorescence signals, and bleaching of the fluorescein rings was not observed during the hour-long experiments.
Flexible electronics make their way into the operating room
The researchers conclude that these first steps towards optical navigation of the DROP-IN gamma probe could further integrate interventional nuclear medicine into robotic surgery. The first application could be in prostate cancer treatments, where robotic surgery is already well established, says van Oosterom. He notes that radio-guided surgery using a radiotracer that targets prostate specific membrane antigen (PSMA), is particularly promising. “The DROP-IN gamma probe allows the surgeon to operate on these patients with the robot, to specifically excise tumour cells using the PSMA-targeted tracer,” he explains.
The team has already demonstrated that the DROP-IN works well for robot-assisted radio-guided lymph node dissection in prostate cancer surgery, as described in European Urology. “Following our successful proof-of-concept studies, we are currently extending in-human trials that evaluate the PSMA-targeted robotic surgery,” van Oosterom tells Physics World. “Current findings suggest that our optical navigated DROP-IN gamma probe setup will provide additional value in these in-human studies.”