Traumatic brain injury is a major cause of death and disability. When a patient attends an A&E or neurocritical care unit with a head injury, one of the most important parameters to assess injury severity is intracranial pressure (ICP), as raised ICP is particularly associated with poor outcome. Measuring ICP, however, is currently a highly invasive process.
Speaking at the recent IOP symposium “Optics in Clinical Practice”, Panicos Kyriacou from the Research Centre for Biomedical Engineering at City, University of London described his team’s work in designing a non-invasive optical sensor technology for dynamically measuring ICP.
Measurement of ICP requires a surgeon to drill a hole in the patient’s skull and insert a pressure transducer (the ICP bolt). As well as being one of the most invasive non-therapeutic procedures, it cannot be performed at the site of an accident and carries large associated risks. “Stabbing a transducer into your brain carries certain risks – haemorrhage, leakage of cerebrospinal fluid or infection – and requires an expert neurosurgeon to perform the procedure. There needs to be a measured decision as to whether a patient really needs an ICP bolt,” Kyriacou explained.
As such, much research effort is now underway to develop methods for non-invasive ICP (nICP) monitoring. Currently, however, there is not a practical dynamic measurement that can rapidly determine absolute ICP values in mmHg.
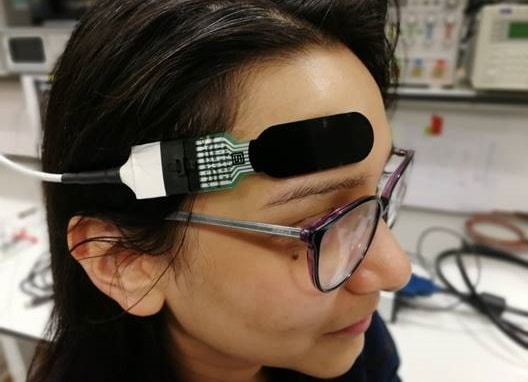
“Our vision is to have a standalone ICP monitor that is completely non-invasive. Such a device will be placed on the forehead and will continuously monitor ICP in absolute numbers, as well as providing graphical ICP trends during monitoring,” said Kyriacou. “The vision of this research is to create a disruptive technology that will replace the most invasive monitor in clinical practice.”
Optical sensing
To create the nICP detector, Kyriacou and colleagues, along with clinical partners from the Royal London Hospital, developed an optical sensor based on photoplethysmography (PPG), which uses light to measure variations in blood volume. The device emits near-infrared light at various wavelengths into the skull and the reflected optical signals are detected by proximal and distal photodiodes. The proximal photodiode detects superficial PPG signals arising from layers of the forehead or scalp. These can be subtracted from the PPG signals read by the distal photodiode, which detects photons from deeper into the brain.
As a first step in evaluating the developed sensor technology and the capability of the acquired optical signals to reflect changes in ICP, the research team performed an in vitro evaluation using a custom made brain phantom. Kyriacou explained that this was a necessary step, as “obviously, we couldn’t recruit volunteers and put bolts in their heads to evaluate the sensor prior to clinical trials”.
The researchers created a brain phantom incorporating vessels with pulsatile flow and contained within a chamber (representing the scalp) that could be pressurized. They placed the optical sensor on the top surface of the phantom and raised the pressure inside the chamber from 10 to 40 mmHg (intracranial pressures of interest to neurosurgeons). Altering the pressure resulted in clear changes in the recorded PPGs.
Key to the success of the nICP device is knowing which features in the PPG trace are directly related to changes in ICP. The researchers examined various features and found two that had a large dependence upon the pressure. They then used these two features to create an ICP prediction model.
The team ran the in vitro experiment three times and saw excellent agreement between the nICP and invasive ICP readings, with correlations of 0.95–0.98 and RMS errors of 1.45–3.12 mmHg for the three datasets. These findings gave the team the confidence to perform in vivo tests on healthy volunteers. While there was no gold-standard comparison in this case, they observed promising trends in ICP measured on volunteers during tilting and Valsalva manoeuvres.
Clinical study
In the most recent phase of this work, the researchers joined forces with the Royal London Hospital, which has one of the largest neurological trauma centres in the UK, to begin clinical trials of the nICP device. They recruited patients that had an intracranial bolt (the gold standard for ICP) as part of their routine monitoring. This pilot clinical study, which began in February 2019 (paused earlier this year as the pandemic struck, and since resumed), has so far evaluated 21 of a targeted 40 patients.
Kyriacou shared some early results, noting that “the results were somewhat too good to be true”. A preliminary data analysis from a small group of patients revealed a high correlation between nICP and gold-standard measurements, with an RMS error of 1.98 mmHg. The nICP device showed a sensitivity of 95% and a specificity of 97% at 20 mmHg.
“These preliminary results generated a lot of excitement and enthusiasm. But this is a small group of patients, the robustness and confidence will come when we analyse all 40 patients, we are still recruiting and still analysing data,” Kyriacou concluded, noting that the group is hoping to commercialize the sensor. “Hopefully, we will be able to translate our research and create a tool to be used for patients and improve their quality-of-life.”



