An open and collaborative research culture is essential for advances in one field to inspire and inform progress in other disciplines, argues experimental particle physicist Karol Lang
Breakthrough technologies originally created for the most ambitious experiments in particle physics have often triggered innovations in medical treatment and diagnosis. Advances in accelerators and beamline engineering have aided the development of highly effective strategies for treating cancer, while detectors designed to capture the most elusive particles have offered new ways to view the inner workings of the human body.
In one recent development, a US-based research team led by Karol Lang, an experimental particle physicist at the University of Texas at Austin, has for the first time achieved real-time imaging of the effects of FLASH proton therapy before, during, and after the delivery of the beam. These emerging FLASH treatments administer ultrahigh doses over extremely short timescales, which can effectively eradicate cancer cells while causing less damage to healthy tissue. FLASH treatments require fewer irradiations over shorter treatment cycles, which would allow more patients to benefit from proton therapy and significantly reduce the risk of radiation-related side effects.
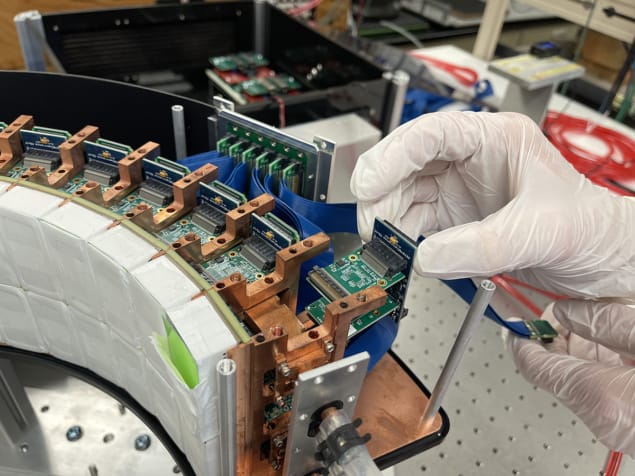
The research team, which also involves medical physicists at the MD Anderson Proton Therapy Center in Houston, produced the images using a purpose-designed scanner for positron-emission tomography (PET), a technique that itself emerged from pioneering experiments at CERN in the 1970s. Using five different phantoms that act as surrogates for a human patient, the team exploited their customized PET instrument to image both the rapid onset of the proton beam and its effects up to 20 minutes after irradiation.
“Irradiation by protons produces short-lived isotopes in the body that in many cases are positron emitters,” explains Lang. “With FLASH proton therapy the beam generates a higher positron intensity, which boosts the strength of the signal. Even with small PET detector arrays we were able to produce images and measure both the abundance of the isotopes and their evolution over time.”
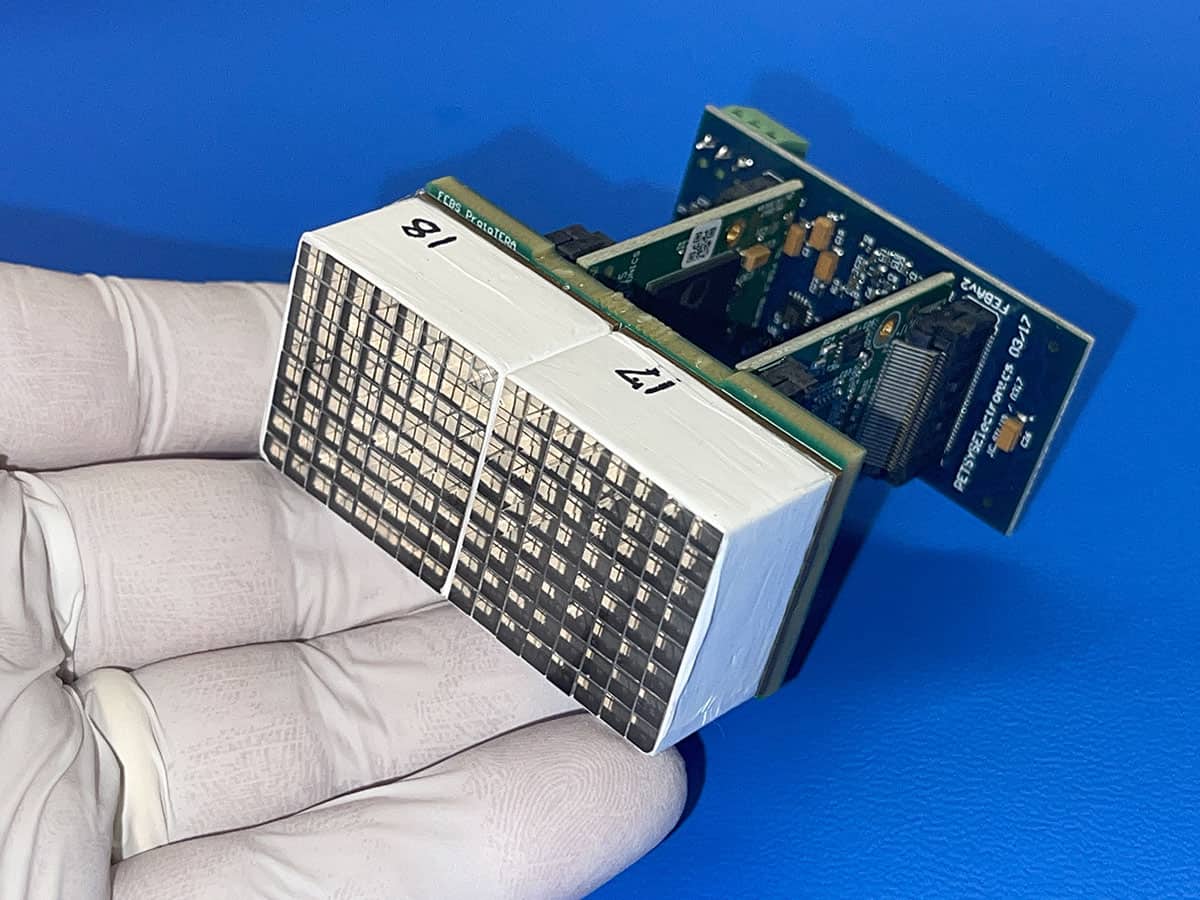
The measurements recorded during these proof-of-principle experiments suggest that an in-beam PET scanner could provide real-time imaging and dosimetry for proton therapy treatments. The team was even able to determine the intensity of the proton beam by detecting prompt gammas – so named because they are produced by the decay of nuclei over very short timescales – produced during the extraction of the proton beam. With just a slight modification of the apparatus, Lang believes that the prompt gammas could be measured to obtain a snapshot of the proton beam, with PET then used to follow the evolution of the isotopes after the beam has been delivered.
“These results show that it would just be a matter of improving the experimental set-up for the technique to provide useful measurements in a clinical setting,” he says. “Of course we know there would still need to be a lot of pre-clinical testing, but at this stage it’s clear that there are no showstoppers for the technique.”
Lang and his colleagues describe their approach and results in two papers published in Physics in Medicine & Biology (PMB), both of which are free to access. The researchers also benefitted from an emerging publishing model, called a transformative agreement, that allowed them to publish both articles open access without needing to pay the usual article publication charges.
Under these so-called transformative agreements, in this case between IOP Publishing and the University of Texas System, researchers at any institution within the academic group can both access research content and publish their own work free of charge. Indeed, IOP Publishing – which publishes PMB on behalf of the Institute of Physics and Engineering in Medicine – now has transformative agreements in place with more than 900 institutions in 33 different countries, providing free access and publishing across most if not all of its portfolio of scientific journals.
The aim of these read-and-publish agreements is to accelerate the transition to open-access publishing, since it avoids the need for researchers to source their own funding for publication charges. For Lang, any move that opens up the science and enables different communities to collaborate will help to trigger new ideas from other disciplines that will drive future innovation. “If I come across an interesting paper that I cannot access, particularly if it is in a different field, I am missing some information that might help me in my work,” he says. “Open and free information is essential for us to make progress.”
From his own experiences in particle physics, Lang has seen the benefits that can emerge from an open and collaborative research culture. “In particle physics everyone shares their best thoughts and achievements, and people want to get involved in finding different ways to develop and exploit new ideas,” he says. “Without that collaborative mindset the breakthroughs we have seen at CERN, Fermilab and elsewhere just wouldn’t have happened.”

However, it is clear that Lang is frustrated that some people in the medical community appear to be less open-minded to new ideas, particularly from a physicist who has no prior clinical experience. “We know that many of the best technologies in medical physics and nuclear imaging come from advances in particle and nuclear physics, but it is hard to bring the latest new ideas into medicine,” he says. “I now understand better why that is – changing tried-and-trusted medical procedures and formal treatment protocols is much more complicated than just swapping in a better detector – but I’m still disappointed at how difficult it is to penetrate the sector and engage in collaborative research.”
While Lang has attempted to build medical detectors before, he acknowledges that he and other particle physicists can be guilty of naivety or even arrogance when it comes to introducing novel technologies into the tightly controlled hospital environment. For this new work, however, a group of medical physicists asked him to take the lead on a research project that required his expertise in building particle detectors. “I’m still continuing my research in neutrino physics, but I believe that what we can offer is so unique and worthwhile that I wanted to get involved,” Lang says. “As I learnt more, I got more intrigued and became really hooked on the idea of FLASH treatments.”
While more work will be needed to optimize the in-beam imaging technique for clinical use, Lang believes that in the short term it could offer a valuable research tool to help understand the FLASH effect. “No-one really knows why FLASH works, or exactly which beam parameters should be used to achieve the best results,” he says. “That suggests to me quite profoundly that we don’t fully understand how radiation interacts with either healthy or cancerous tissue.”
With this new instrument, argues Lang, it would be possible to explore the physical mechanisms at play during a FLASH treatment. “This technique could help us to understand how the human body reacts after it has been irradiated with such intense bursts of energy,” he says. “It offers a way to explore the time-dependent effects of the irradiation, which it seems to me has not been done systematically before.”
Longer term, however, the aim is to create an image-guided treatment modality that would measure the effects of each irradiation to inform and update subsequent treatments. Such adaptive approaches are impractical with conventional treatment protocols, in which smaller doses are delivered in around 30 daily sessions, but could be more viable with FLASH treatments that may only require a few doses to deliver enough energy to eradicate the cancer.
“Checking the effects of each irradiation would completely transform the dynamics, logistics and outcomes of the treatment,” says Lang. “Combined with a better understanding of the interactions between energetic protons and the human body, such adaptive FLASH protocols could have a revolutionary impact on patient outcomes.”



