Cervical cancer is the fourth most common cancer among women globally. According to the World Health Organization, there were an estimated 604 000 new cases and 342 000 deaths in 2020. While surgery and chemotherapy can be used to treat early-stage disease, locally advanced cervical cancer is typically managed with a combination of chemoradiation and brachytherapy.
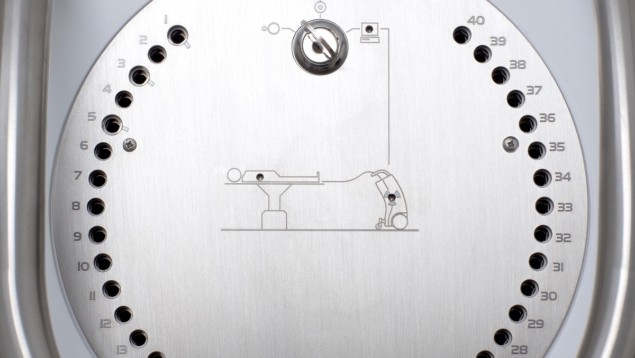
Brachytherapy is a type of radiation therapy in which radioactive sources are placed inside or next to the tumour to deliver a high dose of radiation while minimizing exposure to surrounding healthy tissues. Previous research has demonstrated that for locally advanced cervical cancer, brachytherapy is a key factor for maximizing tumour local control and, hence, overall survival.
Brachytherapy, however, has not undergone the same technological advances as other radiation treatments, with the recommended dosage a one-size-fits-all method. There is a need for customized radiation dose that considers the anatomy of each patient as well as the degree of local tumour dissemination.
One technique that has helped in the targeted administration of radiation is magnetic resonance image-guided adaptive brachytherapy (MR-IGABT). With the assistance of MR images, as well as interstitial needles, MR-IGABT can selectively treat high-risk clinical target volumes (CTVHR). Initial findings from the multicentre EMBRACE-I study established that using MR-IGABT to individualize radiation dose can enhance patients’ overall survival rate, as well as improve local tumour control.
A research group headed up at the Comprehensive Cancer Center of MedUni Vienna and Vienna General Hospital has now carried out a new study using data from the EMBRACE-I study, which included 1318 patients (with a median follow-up of 52 months) from 24 centres across Europe, North America and Asia.
In this latest study, reported in the Journal of Clinical Oncology, the authors aimed to identify the risk factors for local failure (defined as local recurrence or persistence of disease within the treated area) following chemoradiation and MR-IGABT in patients with locally advanced cervical cancer. The researchers analysed various patient-, tumour- and treatment-related factors to identify the predictors of local failure.
The study demonstrated that the use of MR-IGABT was associated with a lower risk of local failure, suggesting that this treatment modality may improve outcomes in patients with locally advanced cervical cancer. Risk factor analysis revealed that tumour histology was one of the most relevant prognostic factors: patients with squamous cell carcinoma had a lower failure risk than those with adeno- or adenosquamous carcinoma. Other parameters with significant impact on local tumour control included maximum tumour dimension, the presence of tumour necrosis, minimal dose to 90% of the CTVHR and a CTVHR volume of larger than 45 cm3.

Brachytherapy proves safe for cervical cancer
The study provides valuable insight into the risk factors for local failure following chemoradiation and MRI-guided brachytherapy. This ability to identify high-risk patient and tumour characteristics could help clinicians tailor treatment strategies for individual parameters (such as histology or tumour size) and improve patient outcome. Importantly, the research also highlights the potential benefits of MR-IGABT, which may offer improved precision in the delivery of radiation therapy and better local control of disease.
One surprising outcome of this investigation was its advocating for a watch-and-wait policy in patients with residual disease, a somewhat counterintuitive approach. Although patients with local failure are often recommended more therapy, the research revealed that 74% of those with local failure achieved remission at a later time without additional treatment. Thus, the use of MR-IGABT may offer improved outcomes in these patients. The researchers say that further research is needed to confirm these findings and to optimize treatment strategies for this patient population.