A plasmonic chip that can diagnose type-1 diabetes (T1D) has been unveiled by researchers at Stanford University in the US. The chip is capable of detecting diabetes-related biomarkers such as insulin-specific autoantibodies and could be used in hospitals and doctors’ surgeries as a quick and simple way to detect early-stage T1D.
Diabetes could affect nearly 370 million people worldwide by 2030, according to the World Health Organization. More worrying still, diabetes is now the second most common chronic disease in children. For reasons that are still unclear, the rate of T1D (also known as autoimmune diabetes) in children is increasing by about 3% every year, with a projected increase of a staggering 70% between 2004 and 2020.
Although T1D was once thought of as being exclusively a childhood disease, around a quarter of individuals now contract it as adults. The rate of type-2 diabetes (T2D) (also called metabolic or diet-induced diabetes), normally seen in overweight adults, has also alarmingly escalated in children since the early 1990s, in part because of the global obesity epidemic. Until quite recently, it was fairly simple to distinguish between T1D and T2D because the diseases had occurred in different groups of people. However, this is becoming more and more difficult because the groups are beginning to overlap. The main problem is that existing diagnostic tests are slow and expensive, and it would be better to detect diabetes as early as possible to ensure the best possible treatment.
Higher concentration of autoantibodies
T1D is different from T2D in that patients with the disorder have a much higher concentration of autoantibodies. These are produced by the body and work against one or more pancreatic islet antigens such as insulin, glutamic acid decarboxylase and/or tyrosine phosphatase. Detecting these autoantibodies, and especially those against insulin (which are the first to appear), is therefore a good way to detect T1D. Again, standard tests are not very efficient and even the most widely used technique, radioimmunoassay (RIA) with targeted antigens, is far from ideal because it is slow and relies on toxic radioisotopes.
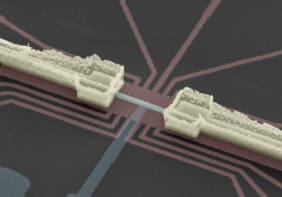
In an attempt to overcome these problems, the Stanford researchers have developed an autoantibody test that is more reliable, simple and faster than RIA and similar tests. It comprises a microarray of islet antigens arranged on a plasmonic gold (pGOLD) chip. It can be used to diagnose T1D by detecting the interaction of autoantibodies in a small blood sample with insulin, GAD65 and IA-2, and potentially new biomarkers of the disease. It works with just 2 µL of whole human blood (from a finger-prick sample, for example) and results can be obtained in the same day.
Enhancing the fluorescence emission
The team, led by Hongjie Dai, made its pGOLD chip by uniformly coating glass slides with gold nanoparticles that have a surface plasmon resonance in the near-infrared part of the electromagnetic spectrum. Plasmons are collective oscillations of the conduction electrons on the surfaces of the nanoparticles. They allow the nanoparticles to act like tiny antennas, absorbing light at certain resonant frequencies and transferring it efficiently to nearby molecules.
The result can be a large boost in the fluorescence of the molecule, and the researchers have shown that the pGOLD chip is capable of enhancing the fluorescence emission of near-infrared tags of biological molecules by around 100 times. Together with Brian Feldman‘s group, the researchers robotically printed the islet antigens in triplicate spots onto the plasmonic gold slide to create a chip containing a microarray of antigens.
“We tested our device by applying 2 µL of human serum or blood (diluted by 10 or 100 times) to it,” explains Dai. “If the sample contains autoantibodies that match one or more of the islet antigens on the chip, those antibodies bind to the specific antigens, which are then tagged by a secondary antibody with a near-infrared dye to make the islet spots brightly fluoresce.”
Antibody detected at much lower concentrations
The samples came from Feldman’s patients who had new-onset diabetes. They were tested against non-diabetic controls at Stanford University Medical Center.
The antigen spots fluoresce 100 times more brightly thanks to the plasmonic gold substrate, which allows the antibody to be detected at much lower concentrations (down to just 1 femtomolar) than if ordinary gold were to be employed in the microarray platform.
“We believe that our technology will be able to address the current clinical need for improved diabetes diagnostics,” Dai says. “The pGOLD platform is also being commercialized by a new start-up company, Nirmidas Biotech, based in San Francisco, aimed at better detecting proteins for a range of research and diagnostic applications. It might even be able to detect biomarkers for other diseases such as heart disease with ultrahigh sensitivity.”
The researchers describe their plasmonic chip in Nature Medicine.
- This article first appeared on nanotechweb.org