Physicians and biomedical engineers at The Ohio State University are exploiting 3D printing technology to help select the optimal valve for a patient receiving an aortic valve replacement. Using CT scans to model the patient’s aorta, they create a 3D-printed replica and use this to predict potential complications – such as leaks, blockages or blood clots – so that they can be avoided.
There are currently two options available for replacing a diseased aortic valve: open heart surgery or a less invasive transcatheter method that deploys a bioprosthetic valve through a blood vessel in the leg. To decide which approach is best for each patient, the researchers create personalized 3D models of the aortic valve and neighbouring structures and investigate how the new valve will function.
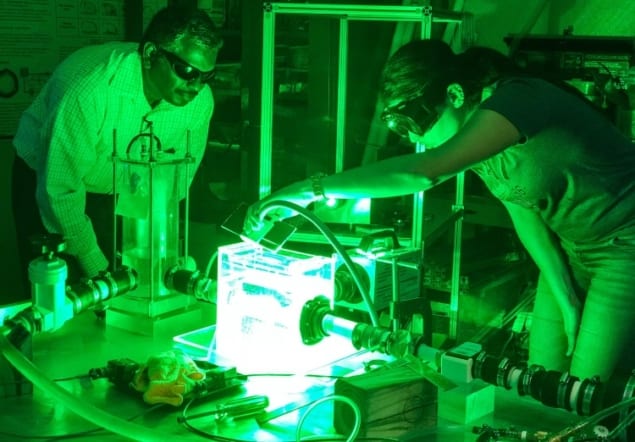
“Using a simulator in a lab, we can replicate what happens in a patient’s left ventricle,” explained Prasad Dasi, a biomedical engineer at The Ohio State University College of Engineering. Dasi’s team precisely reconstruct a patient’s aorta and 3D print it using flexible materials that mimic the aorta. They load the model into a heart simulator that pumps transparent, simulated blood through the system, and then measure blood flow velocity and vortex patterns with and without a replacement valve.
“We can model various therapies, positions and types of valves to better understand problems such as leakage, clotting or coronary obstruction,” Dasi explained. “We can observe how different valves not only relieve the stenosis but also minimize the likelihood of blood clots forming, which is the goal of the treatment.”
At the same time, the team creates computer models to capture the physics of blood flow and interaction between the transcatheter valve and the patient’s anatomy. Long term, their goal is to understand each patient’s unique anatomy and blood flow without performing the physical model experiments, thus speeding the process of personalizing treatment decisions.
“We currently have two valves to choose from in the transcatheter world. I suspect we will have at least four within two years,” said Scott Lilly, interventional cardiologist at The Ohio State Wexner Medical Center. “Each valve is a little different, and the anatomy of every patient is unique. The ability to predict the function of the valve after placement, and which valve may work best with the least amount of leak and without impinging on adjacent structures, is critical.”

Lilly noted that having clinical and biomedical engineering faculty at the same table discussing individual patients makes their heart programme stronger. “In some cases, for example, the coronary arteries come adjacent to where the valve would be placed,” he explained. “Using 3D modelling we can determine whether or not to protect these blood vessels during deployment, or even whether to proceed with valve replacement at all. These discussions have directly informed how we approach many valve replacement procedures.”
Dasi and Lilly are presenting results from this work at the CRT interventional cardiology conference, held this week in Washington, DC.



